Oxidative Stress: And you thought you were stressed!
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
This is part 1 of a series of articles we are posting on Oxidative Stress covering assessing oxidative stress, the importance of glutathione, antioxidants inside and out, the antioxidant effects of cholesterol, and more.
Every single one of your 30 trillion cells is exposed to oxidative stress by the minute and they all need help counteracting it.
The ODX Oxidative Stress Series
- Oxidative Stress part 1 - And You Thought You Were Stressed!
- Oxidative Stress part 2 - Blood Biomarkers: Functional Blood Chemistry Clues
- Oxidative Stress part 3 - Specialized Markers Provide More Clues
- Oxidative Stress part 4 - Cardiometabolic Disease & Oxidative Stress
- Oxidative Stress part 5 - The Cholesterol Connection
- Oxidative Stress part 6 - Glutathione Inside and Out
- Optimal - The Podcast: Episode 1 Oxidative Stress
Oxidative stress occurs when oxidation from free radicals outweighs antioxidant activity in the body, resulting in damage to cells, cell membranes, tissues, and organs. This damage translates into dysregulation of crucial regulatory systems including immune, endocrine, and nervous systems. Over time, oxidative stress can contribute to chronic conditions and disease including:[i] [ii] [iii] [iv] [v] [vi]
- Acute respiratory distress syndrome (ARDs) (associated with low vitamin C and CoQ10)
- Aging effects, sarcopenia, frailty
- Atherosclerosis
- Autoimmune disorders including lupus, rheumatoid arthritis, type 1 diabetes, and scleroderma
- Biliary diseases
- Cancer
- Cardiovascular disease
- Cataracts
- Diabetes
- Insulin resistance
- Macular degeneration
- Metabolic syndrome
- Neurodegenerative diseases
- Respiratory disease
External sources of free radicals include pollution, industrial solvents, radiation, heavy metals, medications, cigarette smoke, alcohol, cooking, and toxins.[vii] For example, mercury can contribute to increased intracellular oxidative stress because it displaces selenium in crucial antioxidant enzymes (e.g. glutathione peroxidase).[viii] Internal sources of free radicals include routine metabolic processes, especially the oxygen-dependent conversion of food to energy.
No matter the source, oxidative stress can damage important molecules including lipids, carbohydrates, protein, and DNA and increase risk of dysfunction and disease.
Key points to remember about oxidative stress:[ix]
- It reflects an imbalance between reactive oxygen species (ROS) and antioxidant activity
- ROS free radicals are generated during normal metabolic processes including mitochondrial production of energy/ATP
- A deficiency of antioxidant defenses will tip the balance in favor of oxidative stress
- Excess ROS is associated with DNA damage and increased risk of chronic diseases such as diabetes, cancer, and cardiovascular disease
- Excess Calorie intake and elevated levels of glucose, free fatty acids, and triglycerides after a meal cause “postprandial oxidative stress” which causes increased mitochondrial and leukocyte generation of ROS
- Cooking quickly at high temperatures increases production of advanced glycation end products (AGEs) which cause endothelial dysfunction and are associated with oxidative stress
- Calorie restriction decreases lipid peroxidation and protein carboxylation
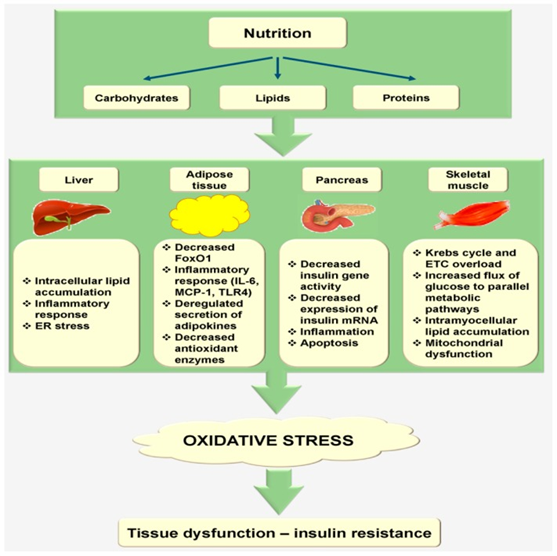
Image reproduced from the following article: Saha, Subbroto Kumar et al. “Correlation between Oxidative Stress, Nutrition, and Cancer Initiation.” International journal of molecular sciences vol. 18,7 1544. 17 Jul. 2017,
So, in closing, be sure not to stress your cells by overeating junk food, exposing them to toxins and pollution, and by having a deficit of antioxidant compounds. Be sure to check out our related posts on assessing oxidative stress, the importance of glutathione, antioxidants inside and out, the antioxidant effects of cholesterol, and more!
Up Next - Oxidative Stress part 2 - Blood Biomarkers
References
[i] Liguori, Ilaria et al. “Oxidative stress, aging, and diseases.” Clinical interventions in aging vol. 13 757-772. 26 Apr. 2018
[ii] Vasdev, Sudesh et al. “Modulation of oxidative stress-induced changes in hypertension and atherosclerosis by antioxidants.” Experimental and clinical cardiology vol. 11,3 (2006): 206-16.
[iii] Cross, C E et al. “Oxidative stress and abnormal cholesterol metabolism in patients with adult respiratory distress syndrome.” The Journal of laboratory and clinical medicine vol. 115,4 (1990): 396-404.
[iv] Girao, H et al. “Cholesterol may act as an antioxidant in lens membranes.” Current eye research vol. 18,6 (1999): 448-54.
[v] Zhang, Bing, and James L Zehnder. “Oxidative stress and immune thrombocytopenia.” Seminars in hematology vol. 50,3 (2013): e1-4.
[vi] Lee, Sun Min et al. “Urinary Malondialdehyde Is Associated with Visceral Abdominal Obesity in Middle-Aged Men.” Mediators of inflammation vol. 2015 (2015): 524291.
[vii] Liguori, Ilaria et al. “Oxidative stress, aging, and diseases.” Clinical interventions in aging vol. 13 757-772. 26 Apr. 2018
[viii] Spiller, Henry A. “Rethinking mercury: the role of selenium in the pathophysiology of mercury toxicity.” Clinical toxicology (Philadelphia, Pa.) vol. 56,5 (2018): 313-326.
[ix] Saha, Subbroto Kumar et al. “Correlation between Oxidative Stress, Nutrition, and Cancer Initiation.” International journal of molecular sciences vol. 18,7 1544. 17 Jul. 2017 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ().






