Welcome to part 8 of the ODX Menopause Series. This post reviews natural approaches to a smooth menopausal transition. These strategies incorporate healthy lifestyle and stress management practices that can be beneficial throughout the lifespan.
The ODX Menopause Series
- Menopause Part 1: A Quick Overview of a Slow Process
- Menopause Part 2: Biology and Physiology of Menopause
- Menopause Part 3: Increased Risk of Disease Associated with Menopause
- Menopause Part 4: Identifying Menopause: Signs and Symptoms
- Menopause Part 5: Laboratory Evaluation of Menopause
- Menopause Part 6: Cardiovascular Risk in Menopause
- Menopause Part 7: Beyond Hormone Testing in Menopause
- Menopause Part 8: Natural Approaches to Menopause
- Menopause Part 9: Diet and Nutrition Intervention in Menopause
- Menopause Part 10: Characteristic of Herbal Derivatives used to Alleviate Menopause Symptoms
- Menopause Part 11: Lifestyle Approaches to Menopause
- Menopause Part 12: The National Institute on Aging Addresses Hot Flashes
- Menopause Part 13: Hormone Replacement Therapy (HRT) in Menopause
- Menopause Part 14: North American and European Guidelines for Hormonal Management of Menopause
- Menopause Part 15: Bioidentical Hormone Therapy
- Menopause Part 16: Optimal Takeaways for Menopause
- Optimal The Podcast - Episode 10
Though hormone replacement therapy tends to be the “go to” in allopathic medicine, it’s possible to resolve some discomfort through more natural means as a first step. It’s equally important to address a menopausal woman’s increased risk of chronic disease by encouraging nutrition and lifestyle patterns that optimize health as well as assist in symptom management.
A 2016 EMAS position statement proposes a holistic framework for the management of a healthy menopause (HM). Healthy diet and lifestyle, physical activity, stress management, and education are the cornerstones of the HM approach. The HM model incorporates a multidisciplinary team that ultimately addresses social and psychological function, as well as physical function and morbidity. A variety of healthcare disciplines should be represented including naturopathic, osteopathic, chiropractic, as well as physiotherapy, homeopathy, and traditional Chinese medicine.[1] Prevention of chronic disease is a significant focus of this holistic approach.
Clearly, menopause can’t be prevented but its negative effects can be managed, and chronic disease risk can be reduced. Basic evidence-based approaches to disease prevention include: [2]
- Alcohol intake moderation
- Exercise
- Healthy diet
- Mental stimulation
- Smoking cessation
- Social engagement
More than half of menopausal women seek complementary and alternative approaches to managing menopause and perceived effectiveness is greater than 60%. Approaches include[3]
|
Mind-body |
Natural products |
Whole system approaches |
|
|
|
DHEA
Dehydroepiandrosterone sulfate, the sulfated form of DHEA, is the most abundant steroid in circulation with levels peaking between 20 and 30 years of age at a level of approximately 370 ug/dL (10 umol/L).[4] It is an important precursor to testosterone and estrogen, including in the postmenopausal period.[5] DHEA supplementation may have a positive effect on body composition, cognitive performance, sexual function, and cardiovascular symptoms though these benefits may vary due to ethnicity.[6]
Schematic overview of the steroid hormone biosynthesis
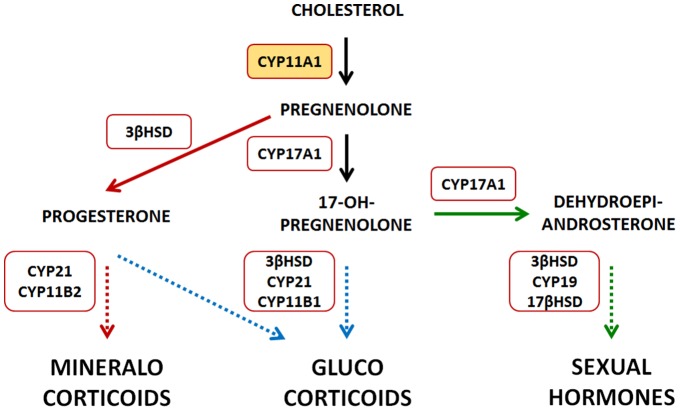
Neunzig, Jens, and Rita Bernhardt. “Dehydroepiandrosterone sulfate (DHEAS) stimulates the first step in the biosynthesis of steroid hormones.” PloS one vol. 9,2 e89727. 21 Feb. 2014, doi:10.1371/journal.pone.0089727 This is an open-access article distributed under the terms of the Creative Commons Attribution License/
DHEAS is the most frequently studied adrenal androgen in perimenopausal studies. Though circulating DHEAS decreases by approximately 80% from age 20 to age 70, it begins to rebound in women transitioning through menopause though levels can decrease again postmenopause. Evaluation of the SWAN study data noted ethnic differences in circulating DHEAS with the highest levels occurring in Chinese subjects, and lowest levels in African American and Hispanic subjects. Higher BMI was associated with lower DHEAS in general. Changes in DHEAS levels correlated with shifts in circulating testosterone and estrogen.[7]
Higher levels of DHEAS were associated with enhanced physical function and quality of life, and fewer symptoms of depression.[8]
According to the position paper of the Polish Menopause and Andropause Society, DHEA supplementation is effective or likely effective in postmenopausal women with:[9]
- Adrenal insufficiency
- Depression and anxiety
- Hypoactive sexual disorder
- Low bone mineral density and/or osteoporosis
- Obesity, insulin resistance
- Vulvovaginal atrophy
- 25-100 mg/day in split doses can be effective, but supplementation is contraindicated in:
- Breast cancer or history of breast cancer
- Vaginal bleeding, untreated endometrial hyperplasia
Research Overview of Natural Approaches to Menopause[10]
- Hypnosis fared well in randomized controlled trials (RCTs) for reducing hot flashes and improving sleep and sexual function and has been recommended by the North American Menopause Society.[11]
- Cognitive-behavioral therapy was effective for reducing the disruptive aspects of hot flashes but not their frequency.
- Relaxation techniques may benefit stress management and vasomotor symptoms, but available research was limited.
- Mindfulness-based stress reduction yielded clinically meaningful improvement in sleep quality, anxiety, perceived stress, and overall quality of life.
- RCTs revealed that practicing yoga significantly reduced symptoms on the Menopause Rating Scale and improved fatigue and overall quality of life.
- Reflexology significantly improved vasomotor and sexual dysfunction symptoms and reduced hot flash frequency by 56% in a 12-week RCT of 120 menopausal women.
- Acupuncture was found to improve somatic, sleep, and vasomotor symptoms in six RCTs of menopausal women.
- Lavender essential oil reduced hot flashes by 50% compared to 1% in the placebo group in a double-blind crossover trial of 100 women.
- Research also demonstrated improvements in sleep, physical, and psychological symptoms using lavender oil.
- Efficacy and benefits of massage were enhanced with the use of aromatherapy as noted in randomized trials.
Herbal therapies
- Black cohosh (Cimicifuga racemose) has been studied for its effects on menopausal symptoms though systematic review of randomized controlled trials found insufficient conclusive evidence for using black cohosh alone. However, one trial that combined black cohosh with St. John’s wort revealed 50% improvement in Menopause Rating Scale scores and significant reductions in depression.
- Wild yam (Dioscorea) has been used in traditional Chinese Medicine for addressing menopausal symptoms, though the amount of clinical research available is limited.
- One randomized controlled study reported 90% improvement in menopausal symptoms (primarily psychological) with the use of 12 grams of Dioscorea alata taken twice daily.
- Dong Quai (Angelica sinensis) has been used in traditional Chinese medicine to address female reproductive issues.
- A randomized controlled study of Dong Quai combined with Matricaria chamomilla demonstrated 90-96% improvement in hot flash frequency and intensity. Dong Quai combined with American ginseng, black cohosh, chasteberry milk thistle, and red clover was associated with a 73% reduction in hot flashes and a 69% reduction in night sweats in a 12-week double-blind placebo-controlled randomized trial of 50 women who also reported improved sleep quality.
- Phytoestrogens found in soy, red clover, hops, flaxseed had mixed results in heterogenous studies. Researchers recommend an expansion of more standardized research to full assess their application in menopause therapy.
- Traditional Chinese medicine herbs had mixed results with some studies reporting improvement in vasomotor symptoms, sexual functioning, tension, insomnia, and depression.
- Additional CAM therapies that warrant further study include Maca (of the brassica family), pollen extract, vitamin E, and homeopathy.
- Review of side effects and contraindications should be integrated into herbal therapy care plans.
Additional Research on Natural Approaches to Menopause:[12]
- Cognitive-behavioral therapy was found to decrease the perceived impact of vasomotor symptoms by 50% with 8 hours of therapy over a 4-6 week period. Positive effects were sustained through at least six months. Although both self-help and group approaches were efficacious in reducing vasomotor symptoms, the in-person group setting was more beneficial in terms of quality of life improvements. The NAMS recommends CBT for vasomotor symptoms.
- Hypnotherapy was associated with a statistically significant decrease in vasomotor symptoms (subjective and objective) following 5 weekly one-hour sessions and some additional “homework.”. An overall 80% reduction in hot flush frequency was reported versus just 15% reduction in controls.
- Mindfulness and relaxation had limited research, however a randomized controlled study of 110 women did not find significant improvement in vasomotor symptoms following 20 hours of mindfulness-based stress reduction.
- A double-blind, randomized controlled trial with 63 women found that the combination of red clover isoflavone and probiotic statistically reduced hot flushes by 4.3 occurrences per day.
- An older review did not find black cohosh efficacious for reducing hot flushes, though a 2020 study used it successfully in combination with 3 other herbs. Women with breast cancer are advised to avoid isoflavones and black cohosh by the NICE guidelines.
- Exercise was not found to specifically improve vasomotor symptoms associated with menopause. However, exercise and yoga were found to improve sleep quality and exercise improved mood.
- Acupuncture was associated with an improvement in vasomotor symptoms that was greater than no treatment at all. However, a randomized trial of 10 consecutive treatments found only a non-statistical benefit of acupuncture versus sham treatment.
References
[1] Stute, Petra et al. “A model of care for healthy menopause and ageing: EMAS position statement.” Maturitas vol. 92 (2016): 1-6. doi:10.1016/j.maturitas.2016.06.018
[2] Lobo, R A et al. “Prevention of diseases after menopause.” Climacteric : the journal of the International Menopause Society vol. 17,5 (2014): 540-56. doi:10.3109/13697137.2014.933411
[3] Johnson, Alisa et al. “Complementary and Alternative Medicine for Menopause.” Journal of evidence-based integrative medicine vol. 24 (2019): 2515690X19829380. doi:10.1177/2515690X19829380
[4] Neunzig, Jens, and Rita Bernhardt. “Dehydroepiandrosterone sulfate (DHEAS) stimulates the first step in the biosynthesis of steroid hormones.” PloS one vol. 9,2 e89727. 21 Feb. 2014, doi:10.1371/journal.pone.0089727
[5] Honour, John W. “Biochemistry of the menopause.” Annals of clinical biochemistry vol. 55,1 (2018): 18-33. doi:10.1177/0004563217739930
[6] Kaya, Cihan et al. “The relation among steroid hormone levels, lipid profile and menopausal symptom severity.” Journal of psychosomatic obstetrics and gynaecology vol. 38,4 (2017): 284-291. doi:10.1080/0167482X.2017.1321633
[7] Lasley, Bill L et al. “The relationship of circulating dehydroepiandrosterone, testosterone, and estradiol to stages of the menopausal transition and ethnicity.” The Journal of clinical endocrinology and metabolism vol. 87,8 (2002): 3760-7. doi:10.1210/jcem.87.8.8741
[8] Santoro, Nanette, and John F Randolph Jr. “Reproductive hormones and the menopause transition.” Obstetrics and gynecology clinics of North America vol. 38,3 (2011): 455-66. doi:10.1016/j.ogc.2011.05.004
[9] Rabijewski, Michal et al. “Supplementation of dehydroepiandrosterone (DHEA) in pre- and postmenopausal women - position statement of expert panel of Polish Menopause and Andropause Society.” Ginekologia polska vol. 91,9 (2020): 554-562. doi:10.5603/GP.2020.0091
[10] Johnson, Aliza et al. “Complementary and Alternative Medicine for Menopause.” Journal of evidence-based integrative medicine vol. 24 (2019): 2515690X19829380. doi:10.1177/2515690X19829380
[11] Johnson, Alisa et al. “Complementary and Alternative Medicine for Menopause.” Journal of evidence-based integrative medicine vol. 24 (2019): 2515690X19829380. doi:10.1177/2515690X19829380
[12] Hickey, Martha, Rebecca A. Szabo, and Myra S. Hunter. "Non-hormonal treatments for menopausal symptoms." bmj 359 (2017).






