Welcome to part 3 of the ODX Stress Biomarkers Series. In this post, the ODX Research team takes a deeper dive into the physiology of stress, including involvement of the brain, adrenal glands, and autonomic nervous system.
The ODX Stress Biomarkers Series
- Stress Part 1: A Quick Overview
- Stress Part 2: How Do We Get Stressed Out?
- Stress Part 3: The Physiology of Stress
- Stress Part 4: Hormonal Control of the Stress Response
- Stress Part 5: Identifying Stress
- Stress Part 6: Disorders Associated with Stress
- Stress Part 7: Biomarkers of Stress Overview
- Stress Part 8: Biomarkers of Stress, Individual Markers
- Stress Part 9: Addressing Stress: Can We Treat It or Beat It?
- Stress Part 10: Nutrition and Stress
- Stress Part 11: Optimal Takeaways
Physiology of Stress
The stress response is physiologically complex and recruits the endocrine, nervous, and immune systems in order to mount an effective adaptive response. While an acute response may keep an organism out of harm’s way, chronic exposure to stress will eventually promote a maladaptive response that disrupts physiology and contributes to cardiovascular disease, gastrointestinal ulcers, immune suppression, sleep dysregulation, and mood and behavioral disorders.[i]
The brain itself is directly affected by stress and the hippocampus, amygdala, and temporal lobe can all be negatively impacted. Chronic exposure to stress hormones can lead to brain atrophy with associated impairment of memory and cognition and even mood disorders. Exposure to synthetic anti-inflammatories may also contribute to hippocampal atrophy and memory dysfunction.[ii]
Once a threat has been perceived, the body goes into overdrive to cope with it and then, ideally, puts on the brakes in an effort to return to normal. Although individuals may respond to stress in different ways, a number of physiological responses are common. The main physiological response to stress increases availability of energy, oxygen, and strength; decreases feeding, appetite, and reproductive physiology; and modulates immune response and function.[iii]
Early on, a cascade of compounds is released via the hypothalamic-pituitary-adrenal (HPA) axis in order to provide resources for the physical stress response. The sympathetic branch of the autonomic nervous system (ANS) then increases heart rate and blood pressure to facilitate fighting or fleeing.[iv] Blood glucose increases as an immediate energy source, and cardiac output and oxygen uptake increase as well in order to facilitate a physical altercation or escape.[v]
Once the threat has passed, the parasympathetic branch of the ANS does its part and opposes sympathetic branch actions, bringing the body back into a balanced state of homeostasis.
This “relaxation response” or “rest and digest” phase will reduce heart rate and blood pressure, slow breathing, and direct blood flow back to internal organs (including digestive organs). Then digestion resumes, sweating diminishes, and blood glucose should come back down to normal levels.[vi]
However, if stress is sustained, then the relaxation response is delayed. The physiological changes associated with adaptation to stress are referred to as allostatic load and include blood pressure, serum glucose, insulin, and lipids, inflammatory markers, and waist circumference. A high allostatic load, representing prolonged stress over time, is reflected in low morning cortisol and reduced cortisol response to stress.
This hypocortisolemic state can be seen in “burnout”, the term often used for excessive stress that leads to exhaustion. Other physiological changes seen with burnout include systemic inflammation, compromised immunity, increased risk of infection, dyslipidemia, and altered glucose regulation. Unhealthy lifestyle habits are also associated with burnout and include reliance on fast food, lack of exercise, and increased consumption of alcohol and pain killers.[vii]
The activation of the hypothalamic-pituitary-adrenal (HPA) axis.
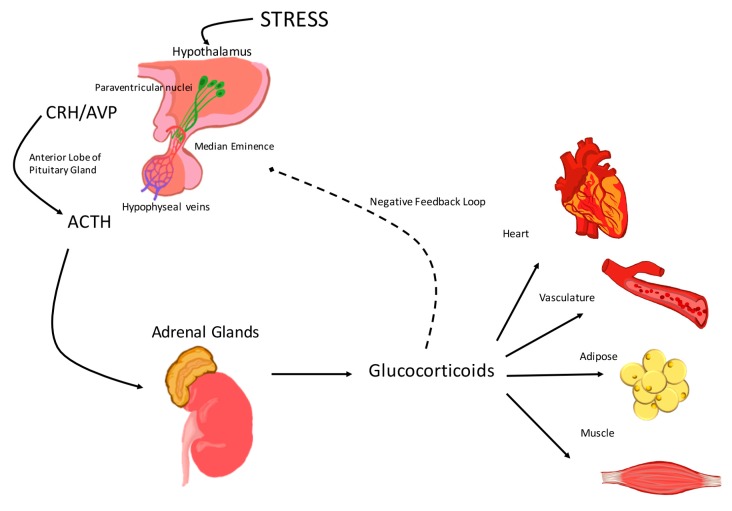
Response to a stress stimulus is routed to the hypophysiotropic neurons in the paraventricular nucleus (PVN) of the hypothalamus. These neurosecretory cells release corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP), which travel through the median eminence and hypophyseal portal vessels. Once CRH reaches the anterior pituitary, it binds CRF type 1 receptors of pituitary corticotroph cells. Adrenocorticotropic hormone (ACTH) is released into circulation, binds its receptors in the zona fasiculata of the adrenal cortex, and causes release of glucocorticoids. Glucocorticoids in circulation act on target cardiovascular tissues (including, the heart, the vasculature, adipose tissue and muscle) then feedback to the level of the central nervous system (CNS) to inhibit activation of the HPA axis.
Source: Burford, Natalie G et al. “Hypothalamic-Pituitary-Adrenal Axis Modulation of Glucocorticoids in the Cardiovascular System.” International journal of molecular sciences vol. 18,10 2150. 16 Oct. 2017, doi:10.3390/ijms18102150 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Ultimately, the physiology of the stress response helps us respond to stress, and then recover from it. If the recovery or “rest and digest” stage is delayed or impeded, then the physiology of stress becomes the stress and the prelude to chronic disease.
References
[i] Chu, Brianna, et al. “Physiology, Stress Reaction.” StatPearls, StatPearls Publishing, 8 June 2021.
[ii] Yaribeygi, Habib et al. “The impact of stress on body function: A review.” EXCLI journal vol. 16 1057-1072. 21 Jul. 2017, doi:10.17179/excli2017-480
[iii] Singh, K. "Nutrient and stress management." J Nutr Food Sci 6.4 (2016): 528.
[iv] Milivojevic, Verica, and Rajita Sinha. “Central and Peripheral Biomarkers of Stress Response for Addiction Risk and Relapse Vulnerability.” Trends in molecular medicine vol. 24,2 (2018): 173-186. doi:10.1016/j.molmed.2017.12.010
[v] Singh, K. "Nutrient and stress management." J Nutr Food Sci 6.4 (2016): 528.
[vi] Murray, Michael T., and Joseph Pizzorno. The encyclopedia of natural medicine third edition. Simon and Schuster, 2012.
[vii] Bayes, Adam et al. “The biology of burnout: Causes and consequences.” The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry vol. 22,9 (2021): 686-698. doi:10.1080/15622975.2021.1907713






