In part 4 of the ODX Insulin Series we take a look at ways you can reverse insulin resistance.
Take a U-Turn and Reverse Insulin Resistance
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
The ODX Insulin Resistance Series
- Insulin Resistance part 1 - The Biochemistry and Physiology of Insulin
- Insulin Resistance part 2 - Insulin Resistance and the Road to Diabetes
- Insulin Resistance part 3 - Assessing Insulin Resistance - Signs, Symptoms & Individual Biomarkers
- Insulin Resistance part 4 - Take a U-Turn and Reverse Insulin Resistance
- Optimal - The Podcast: Episode 3 Insulin Resistance
Insulin resistance and type 2 diabetes do not have to be a one way street or a dead end…
Let’s not forget all of the factors that contribute to insulin resistance and type 2 diabetes in the first
Schematic representation of risk factors for T2DM with convincing or highly suggestive evidence.
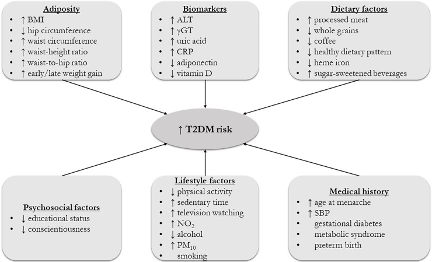
The symbol ↑ denotes a higher exposure to a risk factor, and the symbol ↓ represents a lower exposure to a risk factor. For alcohol consumption, never drinkers presented a higher risk for T2DM than moderate drinkers.
Bellou, Vanesa et al. “Risk factors for type 2 diabetes mellitus: An exposure-wide umbrella review of meta-analyses.” PloS one vol. 13,3 e0194127. 20 Mar. 2018.
What we can do to make that U-turn and reverse course?
It is vitally important to identify blood glucose dysregulation before the pathology of diabetes sets in. Early assessment and intervention is indicated as insulin resistance is associated with abnormal lipid profiles and obesity as early as childhood and adolescence. [1]
In order to reverse insulin resistance, individuals must incorporate habits that are the opposite of habits that cause insulin resistance in the first place.
Basically overeating, especially high-calorie, nutrient-deficient, highly processed foods and resultant obesity, promote insulin secretion and insulin resistance as well as metabolic syndrome and heart disease.
Overeating in general can promote insulin resistance though a variety of factors.
Insulin secretion following a meal will vary depending on meal content, gastrointestinal motility, gastric emptying, and hormonal and neural input following a meal. Ingestion of carbohydrate/glucose, fats/fatty acids, and protein/amino acids can ultimately stimulate insulin secretion. [2] [3] [4] [5]
Intake of animal fat, which is high in saturated fat, appears to be most closely associated with poor glycemic control and diabetes. [6]
A Western-style diet that is highly processed and high in excess fat, animal fat, and carbohydrate can increase risk of insulin resistance, obesity, metabolic syndrome, and type 2 diabetes. However, severe restriction of carbohydrate is not necessarily beneficial as insulin is needed to help suppress endogenous glucose production, a significant factor in insulin resistance. In fact, prolonged carbohydrate restriction can promote hepatic insulin resistance.[7]
However, insulin resistance can be improved and even reversed with a healthy approach to weight reduction, calorie restriction, and regular physical exercise. [8] [9] [10] Elevated blood pressure can also be improved with this approach.
One six-month program studied the effects of lifestyle education and modification on 160 individuals with pre-diabetes (fasting glucose 100-124 mg/dL 5.6-6.9 mmol/L). The study compared a one-time general review of lifestyle changes and prevention of type 2 diabetes…
to a more intensive structured program that incorporated education about pre-diabetes, diabetes, risk factors, and complications, diet improvements, and increased physical activity in the form of lectures and workshops that took place at baseline and again 3 months into the study. [11]
The more intensive interventions induced
- Significant reductions in BMI, fasting glucose, insulin, HOMA-IR, hemoglobin A1C, and total carbohydrate intake; and
- Significant increases in fiber and in micronutrients including vitamins A, C, E, B vitamins, calcium, magnesium, potassium, sodium, copper, iron, and phosphorus.
A healthy approach to weight maintenance will incorporate
- A plant-based diet centered around whole foods
- Abundant intake of fresh fruits and vegetables
- Limited intake of animal-based fats
- Restricting or eliminating processed and canned foods
- Incorporating physically active and structured exercise into one’s daily routine
- Balanced macronutrients, adequate micronutrients
Minerals essential to glucose homeostasis, prevention of type 2 diabetes, and reduction of oxidative stress: [12]
- Boron
- Calcium
- Chloride
- Chromium Cobalt
- Copper Iron
- Iodine
- Magnesium
- Molybdenum
- Phosphorous
- Potassium
- Sodium
- Sulfur
- Zinc
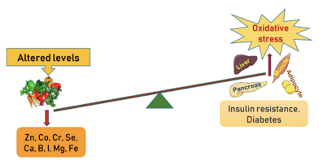
Schematic presentation of the altered levels of trace elements and minerals in the manifestation of oxidative stress in amplifying pathways towards insulin resistance and development of diabetes.[13]
Chromium (trivalent chromium) is a trace element that is appears to be particularly important for glucose tolerance and insulin function. [14]
Researchers note the importance of maintaining chromium sufficiency and recommend replacement in the event of insufficiency. [15] However, some researchers recommended more clinical trials before recommending chromium supplementation. [16]
Other micronutrients that play an integral role in glucose homeostasis include vitamin E (tocopherols and tocotrienols), nicotinamide, B6, B12, folate, and vanadium. [17]
Sufficiency of vitamin D, thiamine, biotin, and vitamin C also appears to be associated with glucose homeostasis. [18]
Omega-3 fatty acids may also play an important role in mitigating insulin resistance and improving glucose metabolism due to their anti-inflammatory actions and support of mitochondrial function. [19]
Ideally adequate amounts of micronutrients can be obtained from the diet. However, if soil depletion, excessive processing, gastrointestinal disorders, or poor diet quality lead to insufficient intake then judicious supplementation may be indicated.
So, the bottom line is, insulin resistance and even pre-diabetes can be rerouted and reversed with diet and lifestyle changes. We just need the will and the way.
Up Next - Optimal - The Podcast: Episode 3 Insulin Resistance
Check out our Series on the HOMA2 Calculator!
References
[1] Ormazabal, Valeska et al. “Association between insulin resistance and the development of cardiovascular disease.” Cardiovascular diabetology vol. 17,1 122. 31 Aug. 2018.
[3] Cen, Jing et al. “Fatty acids stimulate insulin secretion from human pancreatic islets at fasting glucose concentrations via mitochondria-dependent and -independent mechanisms.” Nutrition & metabolism vol. 13,1 59. 30 Aug. 2016.
[4] Wuesten, Oliver et al. “Effects of oral fat load on insulin output and glucose tolerance in healthy control subjects and obese patients without diabetes.” Diabetes care vol. 28,2 (2005): 360-5.
[5] Bisschop, P H et al. “Dietary fat content alters insulin-mediated glucose metabolism in healthy men.” The American journal of clinical nutrition vol. 73,3 (2001): 554-9.
[6] Lichtenstein, A H, and U S Schwab. “Relationship of dietary fat to glucose metabolism.” Atherosclerosis vol. 150,2 (2000): 227-43.
[7] Grandl, Gerald et al. “Short-term feeding of a ketogenic diet induces more severe hepatic insulin resistance than an obesogenic high-fat diet.” The Journal of physiology vol. 596,19 (2018): 4597-4609.
[8] Petersen, Max C, and Gerald I Shulman. “Mechanisms of Insulin Action and Insulin Resistance.” Physiological reviews vol. 98,4 (2018): 2133-2223.
[9] Passa, P. “Hyperinsulinemia, insulin resistance and essential hypertension.” Hormone research vol. 38,1-2 (1992): 33-8.
[10] DeFronzo, R A, and E Ferrannini. “Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease.” Diabetes care vol. 14,3 (1991): 173-94.
[11] Alfawaz, Hanan et al. “Improvements in Glycemic, Micronutrient, and Mineral Indices in Arab Adults with Pre-Diabetes Post-Lifestyle Modification Program.” Nutrients vol. 11,11 2775. 15 Nov. 2019.
[12] Dubey, Pallavi et al. “Role of Minerals and Trace Elements in Diabetes and Insulin Resistance.” Nutrients vol. 12,6 1864. 23 Jun. 2020.
[13] Dubey, Pallavi et al. “Role of Minerals and Trace Elements in Diabetes and Insulin Resistance.” Nutrients vol. 12,6 1864. 23 Jun. 2020.
[14] Linus Pauling Institute Micronutrient Information Center. Chromium. Retrieved October 8, 2020
[15] Prasad, Anisha. "Role of chromium compounds in diabetes." Indian J Pharm Pharmacol 3.1 (2016): 17-23.
[16] Vincent, John B. “Effects of chromium supplementation on body composition, human and animal health, and insulin and glucose metabolism.” Current opinion in clinical nutrition and metabolic care vol. 22,6 (2019): 483-489.
[17] O’Connell, Belinda S. "Select vitamins and minerals in the management of diabetes." Diabetes Spectrum 14.3 (2001): 133-148.
[18] Via, Michael. “The malnutrition of obesity: micronutrient deficiencies that promote diabetes.” ISRN endocrinology vol. 2012 (2012): 103472.
[19] Lepretti, Marilena et al. “Omega-3 Fatty Acids and Insulin Resistance: Focus on the Regulation of Mitochondria and Endoplasmic Reticulum Stress.” Nutrients vol. 10,3 350. 14 Mar. 2018.






