Optimal Takeaways
The free T3 to reverse T3 ratio (FT3:rT3) helps evaluate thyroid hormone conversion and the degree of metabolic stress an individual may be under. A low ratio suggests increased production of reverse T3, which can occur under acute stress, including trauma, surgery, burns, and critical illness, and may not necessarily indicate thyroid dysfunction. A low ratio may indicate liver inflammation and fibrosis as well, and should be evaluated further. A high ratio is not considered clinically significant. Units for free T3 must be in pg/dL and reverse T3 units in ng/dL to calculate the FT3:rT3 ratio in the ODX software.
Standard Range: 2.00 - 28.00 Ratio (FT3 in pg/dL and rT3 in ng/dL)
The ODX Range: 10.00 – 28.00 Ratio (FT3 in pg/dL and rT3 in ng/dL)
Low FT3:rT3 ratio can be associated with severe stress, critical illness, infection, starvation, liver dysfunction (Pagana 2021, Ganesan 2022), oxidative stress, compromised antioxidant status (Mancini 2016), more severe heart failure (Pimental 2009), diabetes, inflammation (Moura Neto et al. 2016), hepatic inflammation (Harrison 2021), and liver fibrosis (Hatziagelaki 2022).
High FT3/rT3 ratio isn’t considered clinically significant.
Overview
Production of reverse T3, a metabolically inactive form of thyroid hormone, often increases during times of stress such as trauma, major surgery, severe infection, burns, critical illness, starvation, liver dysfunction, and chronic stress. The phenomenon of increased reverse T3, low free and total T3, and low or normal T4 and TSH, without thyroid disease, may be referred to as sick euthyroid syndrome (SES) or non-thyroidal illness syndrome. It is associated with transient alterations in the hypothalamus-pituitary-thyroid axis versus true thyroid dysfunction. In such cases, there is less T4 to T3 conversion in the liver and increased conversion of T4 to reverse T3 in the periphery (Pagana 2021, Ganesan 2022). This action reduces metabolic activity and conserves energy as the body fights the stressor.
As the production of reverse T3 increases, levels of metabolically active T3 decline, creating a decrease in the ratio of free T3 to reverse T3 (FT3:rT3). The shift in T3 and reverse T3 production is attributed to deiodinase enzyme activity alterations (Moura Neto and Engelbrecht Zantut-Wittmann 2016). It is essential to recognize that these changes may be due to factors other than thyroid disease and may not require thyroid medication.
Elevated reverse T3 may be considered a marker of hepatic inflammation, and the ratio of free T3 to reverse T3 may decrease as liver fibrosis increases in non-alcoholic steatohepatitis (Harrison 2021). A declining ratio may also help determine the degree of fibrosis in non-alcoholic fatty liver disease (Hatziagelaki 2022).
Thyroid abnormalities are commonly observed in diabetes mellitus, including SES. Research suggests that alterations in T3 and reverse T3 in diabetes may be related to low-grade systemic inflammation. A cross-sectional study of 258 subjects observed a significantly decreased FT3:rT3 ratio in both type 1 and people with type 2 diabetes versus controls, an effect associated with increased inflammatory cytokines. Type 1 diabetics had significantly higher hs-CRP than controls and type 2 diabetics had higher serum amyloid A and significantly higher IL-6 than controls. Researchers suggest anti-inflammatory intervention may help prevent sick euthyroid syndrome in non-thyroid patients (Moura Neto, et al. 2016).
A decreased FT3:rT3 ratio may be an indicator of myocardial dysfunction as well. Evaluation of 46 heart failure patients found that the most severe forms of heart failure were associated with a significantly increased reverse T3 and a significantly decreased FT3:rT3 ratio (Pimental 2009).
Proposed model of the interrelationships between inflammation,
oxidative stress, and thyroid derangement.
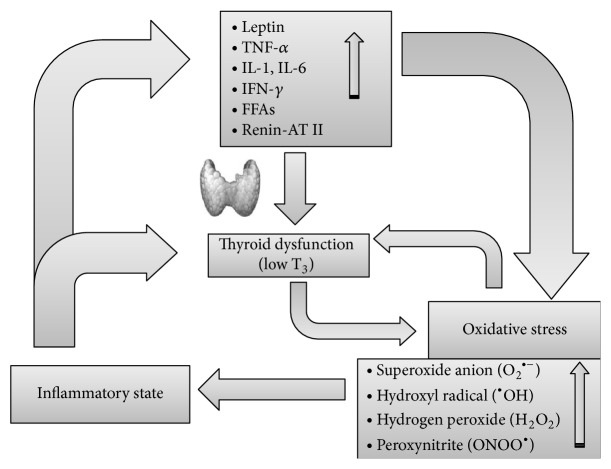
Inflammation, via hormone and cytokine changes, leads to oxidative stress and also affects thyroid function, causing nonthyroidal illness syndrome or pituitary-thyroid axis depression. At the tissue level, hypothyroidism reinforces the oxidative stress, which in turn worsens hypothyroidism by inhibiting deiodinases, thus establishing a vicious circle (see text for further explanations). AT: angiotensin; FFAs: free fatty acids; IFN: interferon; IL: interleukin; TNF: tumor necrosis factor.
Source: Mancini, Antonio et al. “Thyroid Hormones, Oxidative Stress, and Inflammation.” Mediators of inflammation vol. 2016 (2016): 6757154. doi:10.1155/2016/6757154 This is an open access article distributed under the Creative Commons Attribution License
References
Ganesan, Kavitha, et al. “Euthyroid Sick Syndrome.” StatPearls, StatPearls Publishing, 27 October 2022.
Harrison, Stephen A., et al. "Effects of Resmetirom on Noninvasive Endpoints in a 36‐Week Phase 2 Active Treatment Extension Study in Patients With NASH." Hepatology communications 5.4 (2021): 573-588.
Hatziagelaki, Erifili et al. “NAFLD and thyroid function: pathophysiological and therapeutic considerations.” Trends in endocrinology and metabolism: TEM vol. 33,11 (2022): 755-768. doi:10.1016/j.tem.2022.08.001
Mancini, Antonio et al. “Thyroid Hormones, Oxidative Stress, and Inflammation.” Mediators of inflammation vol. 2016 (2016): 6757154. doi:10.1155/2016/6757154
Moura Neto, Arnaldo, and Denise Engelbrecht Zantut-Wittmann. “Abnormalities of Thyroid Hormone Metabolism during Systemic Illness: The Low T3 Syndrome in Different Clinical Settings.” International journal of endocrinology vol. 2016 (2016): 2157583. doi:10.1155/2016/2157583
Moura Neto, Arnaldo et al. “Relation of thyroid hormone abnormalities with subclinical inflammatory activity in patients with type 1 and type 2 diabetes mellitus.” Endocrine vol. 51,1 (2016): 63-71. doi:10.1007/s12020-015-0651-5
Pagana, Kathleen Deska, et al. Mosby's Diagnostic and Laboratory Test Reference. 15th ed., Mosby, 2021.
Pimentel, Carlos Roberto Alves et al. “Reverse T3 as a parameter of myocardial function impairment in heart failure.” International journal of cardiology vol. 145,1 (2010): 52-3. doi:10.1016/j.ijcard.2009.04.001







