Welcome to part 3 of the ODX series on "Biological Age: A True Measure of Health." In the third post in our series, we will discuss the key biomarkers used to measure biological age.
The ODX Biological Age Series
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
- Biological Age - Part 1: What is Biological Age?
- Biological Age - Part 2: How to Measure Biological Age: Overview
- Biological Age - Part 3: How to Measure Biological Age: Key Biomarkers
- Biological Age - Part 4: How to Measure Biological Age: DNA Methylation (DNAm)
- Biological Age - Part 5: How to Measure Biological Age: Telomere Length
- Biological Age - Part 6: How to Improve Biological Age
- Biological Age - Part 7: Optimal Takeaways
Researchers identified a pattern of blood biomarkers that considers physiological processes and changes contributing to aging and disease susceptibility. This set of biomarkers reflects physiological function and biological age and can help predict 10-year mortality. Biological age may also be known as “phenotypic age” or “PhenoAge.”
The biomarkers measured assess the physiological state of various systems, including cardiovascular, liver, kidney, immune, and metabolic systems. Evaluating biomarkers associated with physiological aging and dysfunction can help predict individual differences in cause-specific mortality, all-cause mortality, physical function, cognitive performance, facial aging, and remaining life expectancy. This evaluation is more reflective of true health than chronological age. Researchers reveal that the nine-biomarker panel biological age evaluation was superior and most predictive of (Levine 2023, Levine 2018):
- Lifespan years remaining
- Accumulation of chronic diseases
- Changes in physical and cognitive function
- Pro-inflammatory processes
- Accelerated aging in those with obesity or metabolic syndrome
- Higher biological age in those with Parkinson’s, Alzheimer’s, breast cancer, and HIV
Biological age predicted 10-year survival with 90% accuracy using the epigenetic clock based on these nine biomarkers (Levine 2023, Levine 2018):
- Fasting glucose: Reflects metabolic health
- C-reactive protein (CRP): Reflects inflammation
- Albumin: Reflects liver function, inflammation, malnutrition
- Alkaline phosphatase: Reflects liver function
- Creatinine: Reflects kidney function
- Red Cell Distribution Width (RDW): Reflects immune and hematological function
- Lymphocyte %: Reflects immune function
- White Blood Cell count (WBC): Reflects immune function
- Mean Corpuscular Volume (MCV): Reflects hematological function
The same nine-biomarker pattern was used to determine the biological age of 9,926 subjects from the third National Health and Nutrition Examination Survey (NHANES III). Measurement units for the nine biomarkers that reflect physiological health include (Levine 2018):
- Albumin g/L
- Alkaline phosphatase U/L
- Creatinine umol/L
- CRP mg/dL
- Glucose, serum, mmol/L
- Lymphocyte %
- MCV fL
- Red cell distribution width (RDW) %
- White blood cell count (WBC) 1000 cells/uL
The validity of this calculation for estimating morbidity and mortality was confirmed in NHANES IV. Follow-up confirmed that for each one-year increase in biological age, the risk of:
- All-cause mortality increased by 9%
- Mortality from aging-related diseases increased by 9%
- CVD mortality increased by 10%
- Cancer mortality increased by 7%
- Diabetes mortality increased by 20%
- Mortality from chronic lower respiratory disease increased by 9%
Retrospective calculation of biological age using the nine established biomarkers revealed a strong association between biological age and all-cause mortality in 609 multivessel coronary artery disease PCI patients. Each 10-year increase in biological age correlated with a 51% increase in mortality risk. Researchers note those with a higher biological age had more disease comorbidities (Ma 2022).
A biological age higher than chronological age helped differentiate non-survivors from survivors in a retrospective study of 2,950 critically ill hospitalized patients. Being phenotypically older was associated with an increased risk of mortality. This effect was “accelerated” in those with pre-existing chronic conditions, including cardiovascular disease, end-stage renal failure, diabetes mellitus, cirrhosis, immune disease, or those undergoing immunosuppressive therapy (Ho 2023).
Factors affecting biological age
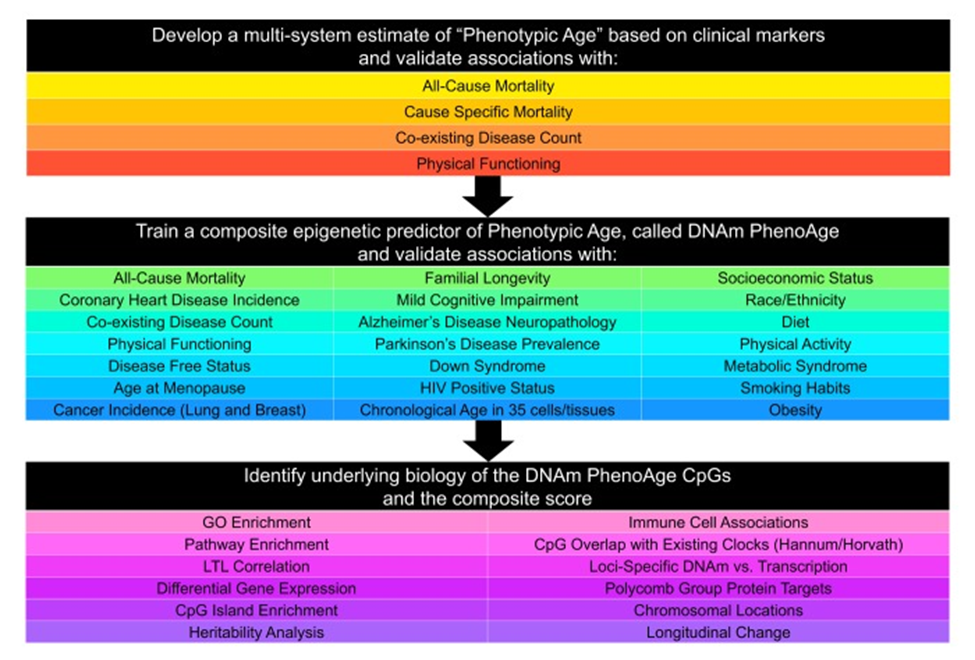 Source: Levine, Morgan E et al. “An epigenetic biomarker of aging for lifespan and healthspan.” Aging vol. 10,4 (2018): 573-591. doi:10.18632/aging.101414 https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/29676998/ This is an open-access article distributed under the terms of the Creative Commons Attribution (CC BY) 3.0 License
Source: Levine, Morgan E et al. “An epigenetic biomarker of aging for lifespan and healthspan.” Aging vol. 10,4 (2018): 573-591. doi:10.18632/aging.101414 https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/29676998/ This is an open-access article distributed under the terms of the Creative Commons Attribution (CC BY) 3.0 License
Physiological Function and Deterioration
The nine biomarkers used to calculate biological age reflect crucial physiological changes associated with inflammation, impaired glucose regulation, compromised liver and kidney function, malnutrition, hematological alterations, and immune competence.
Calculating, addressing, and improving biological age can help reduce the risk of chronic disease and increase the likelihood of a longer healthspan.
References
Ho, Kwok M et al. “Biological age is superior to chronological age in predicting hospital mortality of the critically ill.” Internal and emergency medicine vol. 18,7 (2023): 2019-2028. doi:10.1007/s11739-023-03397-3
Levine, Morgan E et al. “An epigenetic biomarker of aging for lifespan and healthspan.” Aging vol. 10,4 (2018): 573-591. doi:10.18632/aging.101414 This is an open-access article distributed under the terms of the Creative Commons Attribution (CC BY) 3.0 License.
Levine, Morgan. True Age: Cutting-edge Research to Help Turn Back the Clock. Penguin, 2023.
Ma, Qiong et al. “Association between Phenotypic Age and Mortality in Patients with Multivessel Coronary Artery Disease.” Disease markers vol. 2022 4524032. 13 Jan. 2022, doi:10.1155/2022/4524032







