Welcome to part 5 of the ODX "Deep Dive Into Iron Metabolism" Series. In the 5th post in our series, we cover the biomarkers of iron status.
The ODX Iron Metabolism Series
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
- Iron Metabolism Part 1 - Introduction to Iron Metabolism
- Iron Metabolism Part 2 - The physiology of iron
- Iron Metabolism Part 3 - Disorders associated with altered iron status: Iron Deficiency Anemia
- Iron Metabolism Part 4 - Disorders associated with altered iron status: Iron Overload
- Iron Metabolism Part 5 - Biomarkers of iron status
- Iron Metabolism Part 6 - Addressing disorders associated with altered Iron status
- Iron Metabolism Part 7 - ODX Optimal Takeaways and References
Biomarkers of Iron Status
Evaluation of iron blood biomarkers is essential for assessing iron status, diagnosing iron-related disorders, and monitoring iron supplementation or therapy.
Identifying the early stages of both iron insufficiency and overload is crucial to preventing the progression of potentially life-threatening changes in iron status.
- Iron, serum
- Ferritin
- Transferrin
- Transferrin saturation
- Iron-binding capacity
- Hemoglobin
- MCV
- MCH
- RBC size, color
Dynamics of systemic iron balance
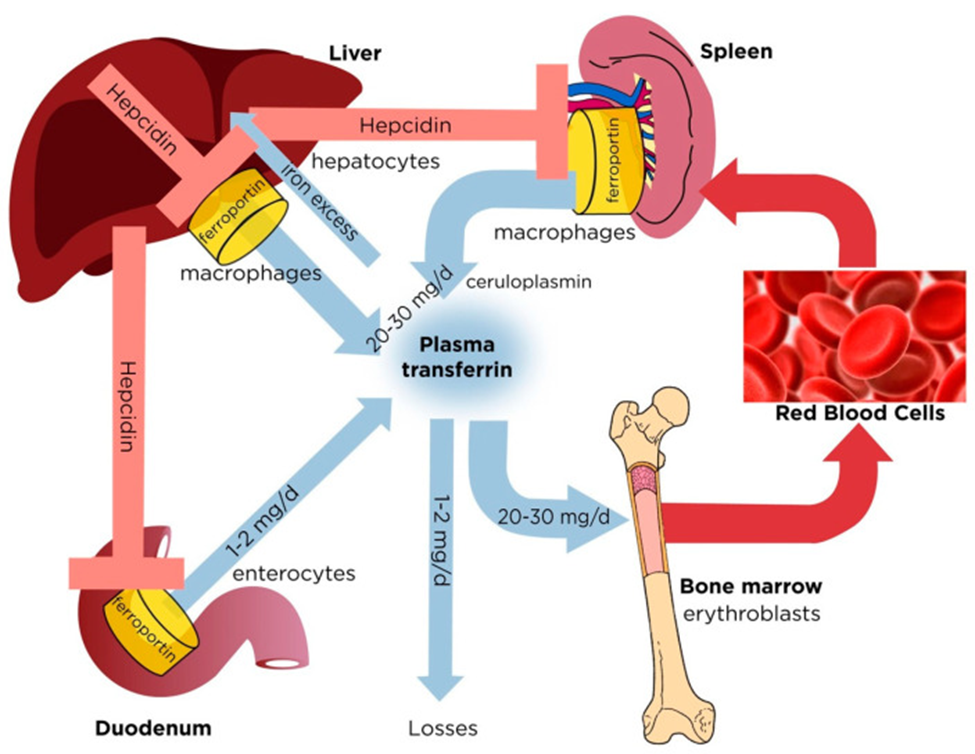
Plasma transferrin delivers iron to bone marrow erythroblasts and to other tissues. It contains a very small (∼0.1%) but highly dynamic fraction of body iron that turns over >10 times/day to meet the iron need for erythropoiesis (20–30 mg/day). The transferrin iron pool is primarily replenished with iron recycled from hepatic and splenic macrophages during erythrophagocytosis of senescent red blood cells. Duodenal enterocytes absorb dietary iron and release small amounts (1–2 mg/day) to compensate for non-specific losses. Hepatocytes store excess of body iron, which can be mobilized to plasma under iron deficiency. Iron efflux to plasma from macrophages, enterocytes or hepatocytes is negatively regulated by hepcidin, a liver-derived peptide hormone that binds to the iron exporter ferroportin and promotes its degradation
Source: Holbein, Bruce E, and Christian Lehmann. “Dysregulated Iron Homeostasis as Common Disease Etiology and Promising Therapeutic Target.” Antioxidants (Basel, Switzerland) vol. 12,3 671. 9 Mar. 2023, doi:10.3390/antiox12030671. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Iron Biomarker Overview
(Gattermann 2021, Pagana 2022, Camaschella 2015, Kotze 2009, Raymond 2021, Yu 2022, McDowell 2022)
Iron, serum
- Serum iron is the amount bound to transferrin in circulation.
- Serum iron decreases with iron deficiency after the first stage of deficiency and increases with iron overload.
- Elevated serum iron is associated with hemochromatosis and may be associated with an increased risk of hepatocellular carcinoma in those with NAFLD without hemochromatosis.
Ferritin
- Ferritin is the major iron storage protein in the body. The amount found in circulation reflects the amount of iron in storage.
- Ferritin decreases with iron deficiency anemia.
- Ferritin increases with iron overload, hemosiderosis, hemochromatosis, megaloblastic anemia, hemolytic anemia, and chronic liver disease.
- Ferritin can act as an acute phase reactant and increase with inflammation, unrelated to iron status.
- Serum ferritin above 300 ng/mL in men and above 150 ng/mL in menstruating females suggests iron overload.
- Levels above 1000 ng/mL significantly increase the risk of liver damage and reduce life expectancy (McDowell 2022).
Transferrin
- Transferrin is the principal iron-binding protein in the blood.
- Transferrin increases when iron stores are low and decreases when too much iron is available.
- The amount of transferrin available for binding iron is reflected in transferrin saturation and iron-binding capacity measurements.
- Transferrin may decrease with acute inflammation, chronic illness, malignancy, liver disease, and collagen vascular diseases (Pagana 2022).
Transferrin saturation
- Transferrin saturation reflects how much transferrin in circulation is saturated with iron.
- Under normal circumstances, approximately 30% of transferrin in circulation is saturated with iron.
- Transferrin saturation decreases below 20% with iron deficiency and increases above 40% with iron overload.
- Fasting transferrin saturation above 60% in men or 50% in women suggests hemochromatosis (Kotze 2009).
Iron-binding capacity
- Serum iron-binding capacity is usually measured by the total iron-binding capacity (TIBC).
- Although the TIBC reflects all serum proteins available for binding iron, it primarily reflects transferrin, the principal iron-binding protein.
- TIBC increases with iron deficiency anemia and decreases with iron overload.
- Iron-binding capacity may be expressed as unsaturated iron-binding capacity (UIBC).
Hemoglobin
- Hemoglobin is a red blood cell protein.
- The iron in hemoglobin binds oxygen and facilitates its delivery throughout the body. It also binds carbon dioxide and facilitates its delivery to the lungs for removal.
- A deficiency of iron leads to a reduction in hemoglobin production, resulting in microcytic (small), hypochromic (pale) red blood cells and diminished oxygen-carrying capacity.
- Hemoglobin measurement is essential for diagnosing iron deficiency anemia. though it is not specific as a stand-alone biomarker.
- It is affected late in the process of IDA and may remain within normal range despite iron insufficiency. It can also be affected by other types of anemia.
MCV
- The mean corpuscular volume (MCV) reflects the average size or volume of red blood cells in circulation.
- Although MCV can remain within range with iron deficiency, it will decrease below 80 fL with IDA (Camaschella 2015).
MCH
- Mean corpuscular hemoglobin (MCH) reflects the average amount of hemoglobin in a red blood cell.
- Although MCH can remain within range with iron deficiency, it will drop below 27 pg with IDA (Camaschella 2015).
Red Cell Distribution Width (RDW)
- The RDW is based on RBC and MCV and reflects variations in the size of red blood cells in circulation.
- RDW is increased with a deficiency of iron, B12, or folate, and related anemias.
Genetic testing for hemochromatosis
- HFE gene mutations with the highest risk of hemochromatosis include C282Y/C282Y, H63D/H63D, or C282Y/H63D.
Additional biomarkers proposed in IDA
(Abbaspour 2014, Camaschella 2015, Pagana 2022, Warner 2023)
- Antiparietal cell antibody (APCA): Increased
- Erythropoietin (EPO): Increased
- Hepcidin: Decreased
- Soluble transferrin receptor (sTFR): Increased
- sTFR/log ferritin Index: Above 2
- Zinc protoporphyrin: Increased
- Reticulocyte hemoglobin content: Low
- Perl’s staining of bone marrow for iron: Negative
- Mentor Index (MCV/RBC Index): Increased in iron deficiency, Decreased in thalassemia minor
ODX Guide to Iron Biomarkers
| Iron Deficiency Anemia | Anemia of chronic disease/ inflammation |
Hemolytic Anemia | Iron overload, hemochromatosis | |
| Serum iron | Decreased depending on the stage of IDA | Normal or decreased | Increased | Increased |
| Ferritin | Decreased | Increased | Increased | Increased |
| Transferrin | Increased | Normal or decreased | Decreased | Decreased |
| % Transferrin saturation | Decreased | Normal or decreased | Increased | Increased |
| Iron-binding capacity | Increased depending on the stage of IDA | Normal or decreased | Decreased | Decreased |
| RDW | Increased | Normal or slightly increased | Increased | Normal |
| Hemoglobin | Decreased in the latter stages of IDA | Decreased | Decreased | Normal |
| MCV | Decreased | Normal or decreased | Normal | Increased |
| MCH | Decreased | Normal or decreased | Decreased | Increased |
Sources: Merck Manual IDA iron overload, Raymond 2021, Pagana 2022, Bermejo 2009, Camaschella 2015, Gattermann 2021, Northrop-Clews 2013, Baldwin 2023, Barton 2000, Pfeiffer 2017
NEXT UP: Iron Metabolism Part 6 - Addressing disorders associated with altered Iron status







