Mercury is a highly toxic heavy metal that can have devastating effects on human health.
Despite being a toxin, mercury is used industrially in the manufacture of electronic devices, paints, and fungicides, as well as in waste incineration (Tinggi 2022).
Mercury toxicity varies with the type and dose of exposure, though it is primarily associated with the outgassing of mercury from dental amalgams, consumption of contaminated seafood, coal-burning power plants, mining, industrial contamination, volcanic activity, accidental spills, or occupational exposure. Metallic mercury can be deposited in the brain, thyroid, breast, heart, muscle, adrenal glands, liver, kidney, skin, sweat glands, pancreas, enterocytes, lungs, salivary glands, testes, prostate, placenta, and fetal tissue (Bernhoft 2012).
Assessment
Assessing mercury status can be complex as notable inter-individual variability can occur regarding blood, urine, hair, and other tissue levels following a given exposure (Branco 2017).
Although not conclusive, some blood chemistry changes may be associated with mercury exposure and should be explored further, including
- Low serum selenium (Gropper 2021)
- Low total T3,low free T3 (Raymond 2021, Afrifa 2018)
- Low total T4 (Afrifa 2018)
- Oxidative stress, malondialdehyde (Dalkiran 2021)
- Lower alkaline phosphatase and increased total protein, antinuclear (ANA) and antinucleolar (ANoA) autoantibodies, and pro-inflammatory cytokines (IFN-γ, TNF-α, and IL-1β) (Branco 2017)
- Urine porphyrins, beta2-microglobulin, and N-acetyl-beta-D-glucosaminidase (Nutall 2004)
Mercury toxicity may be associated with:
- Neurotoxicity, teratogenicity, nephrotoxicity, immunotoxicity, and disruption of selenoprotein homeostasis (Branco 2017)
- DNA damage (Xu 2018)
- High blood pressure (Hu 2018)
Laboratory Tests
Recent mercury exposure can be evaluated by measuring blood, hair, and urine levels, though these do not correlate well with total body burden. Also, symptoms may occur despite low mercury levels. Chronic low-grade mercury may not be easily detected but can be associated with weakness, fatigue, anxiety, depression, odd paresthesias, anorexia, weight loss, gastrointestinal disturbances, memory loss, and difficulty concentrating (Bernhoft 2012).
CDC 2018
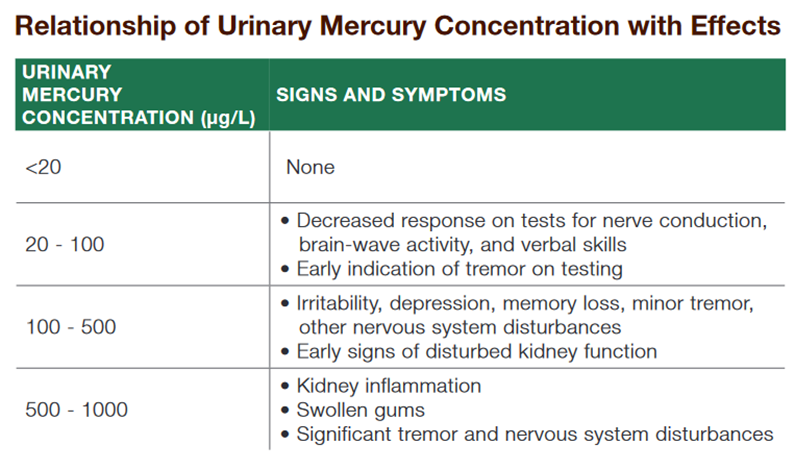
Urine levels of mercury (Hg) provide the most appropriate assessment of elemental mercury exposure and are useful for the assessment of acute and chronic exposures. A 24-hour urine specimen collected in an acid-washed plastic container is the preferred specimen. A first-morning void can provide a close approximation of the urine (using specific gravity or amount of creatinine present).
A urinary mercury concentration of less than 2 micrograms per liter (μg/L) (the 95th percentile for adults) would be considered within the background range.
Mercury has a short half-life in blood (3 days), so blood analysis may be performed during the first 3 days after an acute high-level exposure. Interpretation of blood Hg levels may be complicated by dietary sources of mercury.
Blood samples should be collected in vacutainers containing heparin and then refrigerated.
The blood Hg level for the 95th percentile of the U.S. population is below 5 micrograms per liter (μg/L); a blood concentration of 50 μg/L or greater is considered the threshold for symptoms of toxicity.
Some individuals with high blood mercury levels may not exhibit clinical symptoms. Hair analysis primarily measures organic (methyl) mercury exposure only and is not useful for assessing recent exposures.
Source: CDC. Agency for Toxic Substances and Disease Registry (ATSDR). Evaluating Mercury Exposure: Information for Health Care Providers. October 4, 2018. https://www.atsdr.cdc.gov/dontmesswithmercury/pdfs/info-for-health-care-providers.pdf
Dietary sources of mercury
- Contaminated fish and shellfish (Posin, 2023, Kim 2016)
- High-mercury fish should be minimized or avoided, especially shark, king mackerel, tilefish, swordfish, and tuna. Freshwater fish, including pike, walleye, muskellunge, and bass, should be eaten in moderation only (Posin 2023).
- Contaminated seafood, vegetables, vegetable oil, mixed rice dishes, and liquor may be significant mercury sources (Wells 2020).
Treatment
If mercury overload is confirmed, decontamination should be undertaken and chelation initiated as early as possible to minimize toxic effects. A qualified healthcare practitioner may help facilitate removal using the chelator DMPS for most cases or DMSA for organic mercury (Bernhoft 2012).
Adequate selenium intake may help mitigate mercury toxicity. Primary food sources include Brazil nuts, seeds, mushrooms, fish, seafood, beef, and poultry (Nessel 2023). Selenium content can vary depending on the selenium content of the soil in which foods are grown or grazed. Notable selenium sources include (Tinggi 2022):
|
Food |
Selenium Level (µg/kg) |
Country |
| Milk and dairy products | ||
| Milk | 10.7–16.2 | Greece |
| Milk | 10.0–14.0 | Switzerland |
| Milk | 60.0 | Korea |
| Milk | 22.5–25.9 | Australia |
| Cheese | 24.1–95.4 | Greece |
| Cheese | 70.0–78.9 | Australia |
| Meat and eggs | ||
| Beef | 33.5–6.31 | Greece |
| Beef | 67 ± 23 | Switzerland |
| Beef | 324 | Korea |
| Lamb | 80 | Switzerland |
| Chicken | 76.3–82.4 | Greece |
| Chicken | 114 ± 17 | Switzerland |
| Pork | 90.0–98.2 | Greece |
| Pork | 115 ± 75 | Switzerland |
| Pork | 174–199 | Korea |
| Eggs | 56.4–181.1 | Greece |
| Eggs | 190–414 | Australia |
| Cereals | ||
| Bread | 37.9–150.2 | Greece |
| Bread | 23–48 | Switzerland |
In the United States, the estimated average requirement for selenium for non-pregnant, non-lactating adults is 45 micrograms/day, the RDA is 55 micrograms/day, and the tolerable upper intake level is 400 micrograms/day (Nessel 2023).
Optimal Takeaways
Mercury is highly toxic to humans and can cause irreversible and potentially fatal organ damage. Complete avoidance is the best health policy.- Minimize contaminated vegetables, vegetable oil, mixed rice dishes, and liquors
- Minimize or avoid the most concentrated sources of mercury, including:
- Shark
- King mackerel
- Tilefish
- Swordfish
- Tuna
- Eat freshwater fish, including pike, walleye, muskellunge, and bass in moderation
- Maintain adequate selenium status.
- Chelation by a qualified healthcare professional may be indicated in confirmed cases of toxicity.
References
Afrifa, Justice et al. “Variation in thyroid hormone levels is associated with elevated blood mercury levels among artisanal small-scale miners in Ghana.” PloS one vol. 13,8 e0203335. 30 Aug. 2018, doi:10.1371/journal.pone.0203335
Bernhoft, Robin A. “Mercury toxicity and treatment: a review of the literature.” Journal of environmental and public health vol. 2012 (2012): 460508. doi:10.1155/2012/460508 This is an open access article distributed under the Creative Commons Attribution License,
Branco, Vasco et al. “Biomarkers of mercury toxicity: Past, present, and future trends.” Journal of toxicology and environmental health. Part B, Critical reviews vol. 20,3 (2017): 119-154. doi:10.1080/10937404.2017.1289834
CDC 2018. Agency for Toxic Substances and Disease Registry (ATSDR). Evaluating Mercury Exposure: Information for Health Care Providers. October 4, 2018. https://www.atsdr.cdc.gov/dontmesswithmercury/pdfs/info-for-health-care-providers.pdf
Dalkiran, Tahir et al. “Evaluation of oxidative stress biomarkers in acute mercury intoxication.” Folia medica vol. 63,5 (2021): 704-709. doi:10.3897/folmed.63.e56110
Gropper, Sareen S.; Smith, Jack L.; Carr, Timothy P. Advanced Nutrition and Human Metabolism. 8th edition. Wadsworth Publishing Co Inc. 2021.
Hu, Xue Feng et al. “Mercury Exposure, Blood Pressure, and Hypertension: A Systematic Review and Dose-response Meta-analysis.” Environmental health perspectives vol. 126,7 076002. 31 Jul. 2018, doi:10.1289/EHP2863
Kim, Seong-Ah et al. “Assessment of Dietary Mercury Intake and Blood Mercury Levels in the Korean Population: Results from the Korean National Environmental Health Survey 2012-2014.” International journal of environmental research and public health vol. 13,9 877. 1 Sep. 2016, doi:10.3390/ijerph13090877
Nessel, Trevor A. and Vikas Gupta. “Selenium.” StatPearls, StatPearls Publishing, 3 April 2023.
Nuttall, Kern L. “Interpreting mercury in blood and urine of individual patients.” Annals of clinical and laboratory science vol. 34,3 (2004): 235-50.
Posin, Shawn L., et al. “Mercury Toxicity.” StatPearls, StatPearls Publishing, 8 August 2023. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ),
Raymond, Janice L., et al. Krause and Mahan's Food & the Nutrition Care Process. Elsevier, 2021.
Tinggi, Ujang, and Anthony V Perkins. “Selenium Status: Its Interactions with Dietary Mercury Exposure and Implications in Human Health.” Nutrients vol. 14,24 5308. 14 Dec. 2022, doi:10.3390/nu14245308
Wells, Ellen M et al. “Seafood, wine, rice, vegetables, and other food items associated with mercury biomarkers among seafood and non-seafood consumers: NHANES 2011-2012.” Journal of exposure science & environmental epidemiology vol. 30,3 (2020): 504-514. doi:10.1038/s41370-020-0206-6
Xu, Xijin et al. “Blood concentrations of lead, cadmium, mercury and their association with biomarkers of DNA oxidative damage in preschool children living in an e-waste recycling area.” Environmental geochemistry and health vol. 40,4 (2018): 1481-1494. doi:10.1007/s10653-017-9997-3







