Optimal Takeaways
Asymmetric dimethylarginine (ADMA) is a metabolite of the amino acid arginine that inhibits nitric oxide production and promotes oxidative stress. Elevated ADMA is associated with nitric oxide insufficiency, endothelial dysfunction, cardiovascular and cerebrovascular disease, hypertension, and insulin resistance. Lower levels are associated with improved or optimal cardiometabolic function.
Standard Range: 0.00 – 123.00 ng/mL (0.00 – 0.61 umol/L)
The ODX Range: 0.00 – 100.00 ng/mL (0.00 - 0.50 umol/L)
Low ADMA is associated with a lower risk of endothelial dysfunction, hypertension, and cardiometabolic disease.
High ADMA is associated with cardiovascular disease, cardiometabolic dysfunction, hypertension, atherosclerosis, heart failure, renal failure, diabetes mellitus (Sibal 2010), end-stage renal disease (Oliva-Damaso 2019), endothelial dysfunction, triple vessel CAD, increased risk of myocardial infarction (Goudhaman 2021), free radical production, oxidative stress, inflammatory bowel disease (Nemeth 2017), rheumatoid arthritis (Zafari 2020), insulin resistance (Stuhlinger 2002), obesity associated with insulin resistance (McLaughlin 2006), obesity-related sleep apnea (Arlouskaya 2019), cerebral hypoxia, hypoperfusion, cerebrovascular dysfunction, stroke, Alzheimer’s disease (Khan 2021), hypercholesterolemia, sickle cell disease, systemic lupus erythematous, PCOS, primary dysmenorrhea, and preeclampsia (Tain 2017).
Elevated ADMA and decreased nitric oxide may promote the generation of free radicals, LDL oxidation, vascular inflammation, endothelial cell death, smooth muscle proliferation, and increased platelet adhesion and aggregation (Willeit 2015).
Overview
Asymmetric dimethylarginine (ADMA) is a naturally occurring methylated analog of the amino acid arginine. Although low levels of ADMA may be found normally in circulation, elevated levels can be detrimental and are associated with hypertension, hypercholesterolemia, chronic heart failure, increased carotid intima-media thickness (CIMT), chronic kidney failure, and diabetes mellitus. Endothelial release of ADMA is enhanced in the presence of LDL, whether oxidized or native. Increased ADMA is strongly associated with atherosclerosis and is considered a significant predictor of cardiovascular events and mortality in coronary artery disease (CAD) patients (Sibal 2010).
The adverse effects of ADMA are associated with its inhibition of the enzyme nitric oxide synthase (NOS), the catalyst for converting L-arginine to nitric oxide (NO) and citrulline. ADMA and its enantiomer SDMA uncouple NOS, producing superoxide free radicals instead of nitric oxide and peroxynitrite formed from the combination of superoxide and nitric oxide (Khan 2021).
Nitric oxide is an anti-inflammatory ant-apoptotic molecule that inhibits platelet aggregation, reduces leukocyte adhesion, and helps maintain blood flow (Khan 2021). It is a potent vasodilator that supports endothelial function. Its insufficiency can lead to endothelial dysfunction, one of the earliest signs of atherosclerosis (Goudhaman 2021). Nitric oxide is also a central nervous system neurotransmitter (Appleton 2002).
Elevated ADMA and decreased nitric oxide may promote the generation of free radicals, LDL oxidation, vascular inflammation, endothelial cell death, smooth muscle proliferation, and increased platelet adhesion and aggregation (Willeit 2015). Increasing ADMA levels can be further exacerbated by oxidative stress, which can inhibit DDAH, the enzyme that breaks down ADMA. Therefore, elevated ADMA may indicate existing oxidative stress (Nemeth 2017). Hyperglycemia and angiotensin II administration can also inhibit the enzymes that break down ADMA and contribute to its accumulation. Tissue levels of ADMA can be even higher than circulating levels, though tissue sampling is more invasive and less practical (Tain 2017).
ADMA elevation is considered predictive of future myocardial infarction in those with CAD. A pilot study of 40 subjects with obstructive CAD found that ADMA levels were significantly higher in those with the most severe CAD, i.e., triple vessel disease (TVD). Mean ADMA levels were 167.74 ng/mL (0.83 umol/L) with TVD, 159.46 ng/mL (0.79 umol/L) with double vessel disease, 149.5 ng/mL (0.74 umol/L) with single vessel disease; and 144.54 ng/mL (0.72 umol/L) with mild CAD, i.e., less than 20% stenosis of the coronary artery (Goudhaman 2021).
A meta-analysis of 22 prospective observational studies comprising 19,842 subjects followed over seven years found that the risk of cardiovascular disease was approximately 40% higher in those with ADMA levels in the top third of baseline versus those in the bottom third (Willeit 2015). A meta-analysis comprising 5,528 apparently healthy individuals reported mean plasma ADMA levels ranging from 0.50 ng/mL (100 umol/L) to 147 ng/mL (0.73 umol/L), depending on the method of analysis, i.e., ELISA, LC/MS, or HPLC (Nemeth 2017).
Elevated ADMA is also observed in cerebrovascular disease, neurovascular injury, and pathological states such as Alzheimer's disease and stroke due to accumulation of peroxynitrite and relative insufficiency of nitric oxide. Peroxynitrite can cause blood-brain barrier perforation and leakage, contributing to endothelial dysfunction (Khan 2021).
There is a significant association between ADMA, endothelial dysfunction, and high blood pressure. Researchers hypothesize that ADMA may increase due to an increase in hypertension-induced oxidative stress, which inhibits the breakdown of ADMA or hypertension-induced shear stress on the artery. Also, endothelial dysfunction itself is associated with both hypertension and elevated ADMA. A case-control study of 260 with essential hypertension and 144 controls found that hypertensives had significantly higher serum ADMA with a mean of 163.6 vs. 145.44 ng/mL (0.81 vs. 0.72 umol/L). ADMA levels were significantly higher in hypertensives with diabetes in the study. Researchers note that exogenous arginine can reverse the adverse effects of ADMA on the NOS enzyme, improve endothelial function, and improve outcomes in hypertensive individuals (Gamil 2020).
Arginine is considered a semi-essential amino acid and should be supplemented when endogenous production is insufficient. It has been used therapeutically in hypertension, angina, CHF, CAD, and intermittent claudication based on its NO-stimulating effects (Appleton 2002).
Elevated ADMA is seen with obesity-related insulin resistance, a risk factor for cardiovascular disease. One study recruited “healthy, overweight women interested in weight loss” and found that ADMA levels were significantly higher in those with insulin resistance, i.e., 341.38 ng/mL (1.69 umol/L) versus 238.36 (1.18 umol/L). ADMA decreased to 242.4 ng/mL (1.2 umol/L) when obese insulin-resistant women lost weight. Interestingly, baseline steady-state plasma glucose and fasting plasma insulin were significantly higher in insulin-resistant obese women 241 mg/dL versus 85 mg/dL glucose (13.38 vs. 4.72 mmol/L) and 25.3 vs. 5.3 uU/mL insulin (175.71 vs. 36.81 pmol/L) respectively, but fasting glucose was not significantly different at 103 vs. 93 mg/dL (5.72 vs 5.16 mmol/L) (McLaughlin 2006).
Some plant-based foods contain ADMA, including soybean, rye, sweet peppers, broad beans, and potatoes. Intake of these foods should be considered in individuals with elevated ADMA (Servillo 2013).
ADMA and SDMA metabolism
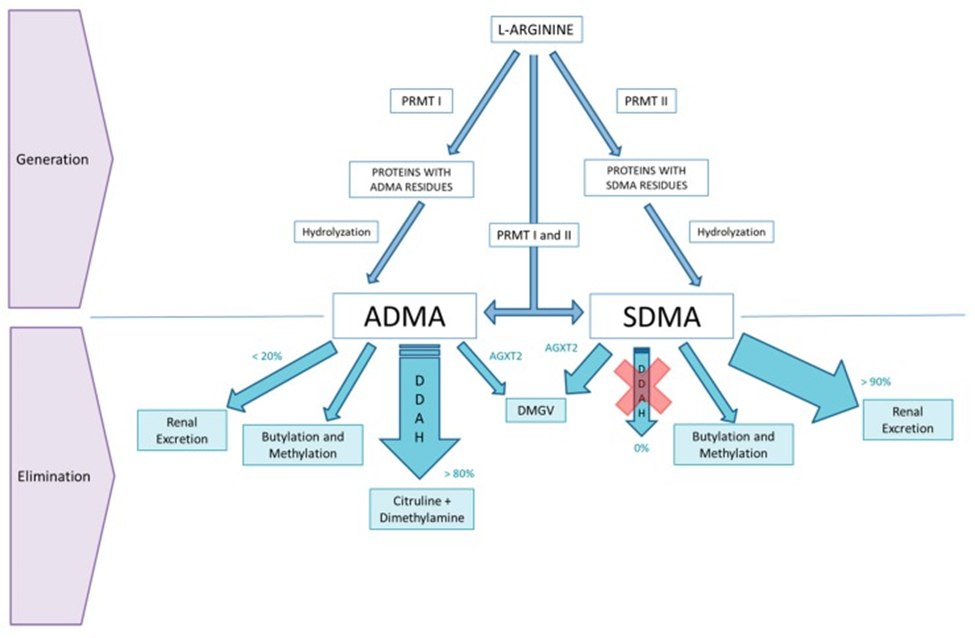
Source: Oliva-Damaso, Elena et al. “Asymmetric (ADMA) and Symmetric (SDMA) Dimethylarginines in Chronic Kidney Disease: A Clinical Approach.” International journal of molecular sciences vol. 20,15 3668. 26 Jul. 2019, doi:10.3390/ijms20153668 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
References
Appleton, Jeremy. “Arginine: Clinical potential of a semi-essential amino acid..” Alternative medicine review : a journal of clinical therapeutic vol. 7,6 (2002): 512-22.
Arlouskaya, Yana et al. “Asymmetric Dimethylarginine (ADMA) and Symmetric Dimethylarginine (SDMA) Concentrations in Patients with Obesity and the Risk of Obstructive Sleep Apnea (OSA).” Journal of clinical medicine vol. 8,6 897. 23 Jun. 2019, doi:10.3390/jcm8060897
Gamil, Sahar et al. “Increased Serum Levels of Asymmetric Dimethylarginine and Symmetric Dimethylarginine and Decreased Levels of Arginine in Sudanese Patients with Essential Hypertension.” Kidney & blood pressure research vol. 45,5 (2020): 727-736. doi:10.1159/000508695
Goudhaman, Lakshmi et al. “Association of Serum Asymmetric Dimethylarginine with the Severity of Coronary Artery Disease: A Pilot Study.” Reports of biochemistry & molecular biology vol. 10,2 (2021): 302-306. doi:10.52547/rbmb.10.2.302
Khan, Mushfiquddin et al. “Asymmetric dimethylarginine-induced oxidative damage leads to cerebrovascular dysfunction.” Neural regeneration research vol. 16,9 (2021): 1793-1794. doi:10.4103/1673-5374.306080
McLaughlin, Tracey et al. “Plasma asymmetric dimethylarginine concentrations are elevated in obese insulin-resistant women and fall with weight loss.” The Journal of clinical endocrinology and metabolism vol. 91,5 (2006): 1896-900. doi:10.1210/jc.2005-1441
Nemeth, Balázs et al. “The issue of plasma asymmetric dimethylarginine reference range - A systematic review and meta-analysis.” PloS one vol. 12,5 e0177493. 11 May. 2017, doi:10.1371/journal.pone.0177493. This is an open access article distributed under the terms of the Creative Commons Attribution License
Oliva-Damaso, Elena et al. “Asymmetric (ADMA) and Symmetric (SDMA) Dimethylarginines in Chronic Kidney Disease: A Clinical Approach.” International journal of molecular sciences vol. 20,15 3668. 26 Jul. 2019, doi:10.3390/ijms20153668
Servillo, Luigi et al. “The methylarginines NMMA, ADMA, and SDMA are ubiquitous constituents of the main vegetables of human nutrition.” Nitric oxide : biology and chemistry vol. 30 (2013): 43-8. doi:10.1016/j.niox.2013.02.080
Stuhlinger, Markus C et al. “Relationship between insulin resistance and an endogenous nitric oxide synthase inhibitor.” JAMA vol. 287,11 (2002): 1420-6. doi:10.1001/jama.287.11.1420
Tain, You-Lin, and Chien-Ning Hsu. Toxic Dimethylarginines: Asymmetric Dimethylarginine (ADMA) and Symmetric Dimethylarginine (SDMA).” Toxins vol. 9,3 92. 6 Mar. 2017, doi:10.3390/toxins9030092
Willeit, Peter et al. “Asymmetric dimethylarginine and cardiovascular risk: systematic review and meta-analysis of 22 prospective studies.” Journal of the American Heart Association vol. 4,6 e001833. 28 May. 2015, doi:10.1161/JAHA.115.001833
Zafari, Parisa et al. “Asymmetric and symmetric dimethylarginine concentration as an indicator of cardiovascular diseases in rheumatoid arthritis patients: a systematic review and meta-analysis of case-control studies.” Clinical rheumatology vol. 39,1 (2020): 127-134. doi:10.1007/s10067-019-04713-z







