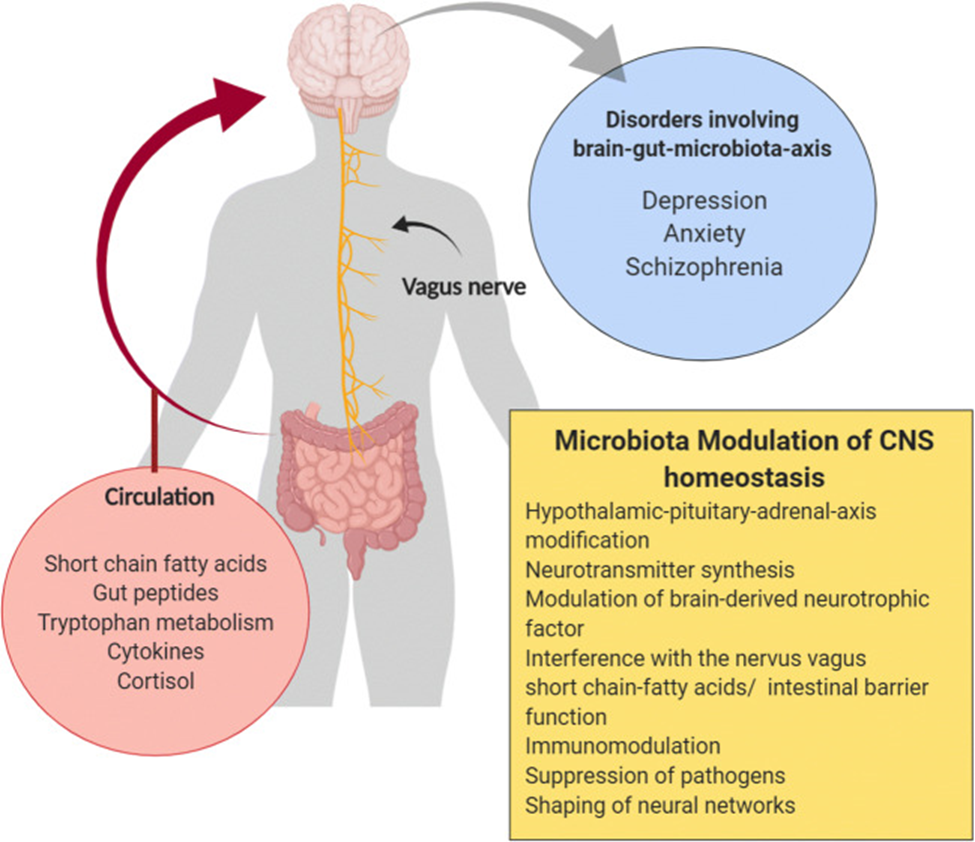
The gut microbiota is a diverse collection of bacteria, viruses, protozoa, archaea, and fungi that live in the human gastrointestinal tract and are essential for many physiological processes. These microorganisms communicate with the peripheral and central nervous systems through the microbiota-gut-brain axis. The exact mechanisms of this communication are still being studied but involve neural, endocrine, and immune pathways. These pathways are often found to be altered in psychiatric disorders.
The gut microbiota can be modified through prebiotics, probiotics, antibiotics, synbiotics, postbiotics, and fecal microbiota transplantation to potentially treat psychiatric disorders, as these approaches are believed to improve mental health through their microbiota-modifying properties.
The primary phylotypes in the gut are called Firmicutes and Bacteroidetes and most studies use Lactobacillus and Bifidobacteria species [though probiotic yeast strains such as Saccharomyces boulardii have also been used.
However, microbial communities are unique to each individual and have specific finger-print-like characteristics. Therefore, the commonly used terms a ‘healthy gut microbiome’ and ‘dysbiosis’ may not be specific or diagnostic.
Probiotics are thought to contribute to a balanced gut environment by suppressing pathogens and interacting with host microbiota.
Source: Mörkl, Sabrina et al. “Probiotics and the Microbiota-Gut-Brain Axis: Focus on Psychiatry.” Current nutrition reports vol. 9,3 (2020): 171-182. doi:10.1007/s13668-020-00313-5 This article is licensed under a Creative Commons Attribution 4.0 International License http://creativecommons.org/licenses/by/4.0/.
The evolving field of nutritional psychiatry should be integrated into clinical practice to treat and prevent psychiatric disorders as well as metabolic comorbidities
Although the therapeutic use of probiotics to support mental health is promising, there are a number of factors that must be considered:
Mörkl, Sabrina et al. “Probiotics and the Microbiota-Gut-Brain Axis: Focus on Psychiatry.” Current nutrition reports vol. 9,3 (2020): 171-182. doi:10.1007/s13668-020-00313-5 T