COVID-19 and chronic disease are close cousins
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
Many of the risk factors observed in more severe COVID-19 overlap those for chronic metabolic diseases.
The ODX COVID-19 Series
- COVID-19: The pandemic that has become endemic
- COVID-19: Overlapping risk factors and chronic disease
- Nutritional status and COVID-19: A covert factor in disease susceptibility
- COVID-19: Blood chemistry biomarker patterns - Clues and patterns lurking just under the surface
- COVID-19: Blood chemistry biomarker patterns - Down the research rabbit hole
- COVID-19: Blood Biomarkers - Neutrophils
- COVID-19: Blood Biomarkers - Albumin
- COVID-19: BloodBiomarkers - Cytokines
- COVID-19: Blood Biomarkers - Interleukin-6
- COVID-19: Blood Biomarkers - Interleukin-10
- COVID-19: Blood Biomarkers - Vitamin C
- COVID-19: Blood Biomarkers - Vitamin D
- COVID-19: Blood Biomarkers - Zinc
- Biomarker characteristics and blood type - help sharpen the COVID-19 clinical picture
- COVID-19: Initial indications and conventional interventions
- COVID-19: Long-term risk reduction - Naturopathic, functional medicine, and nutrition-based approaches to prevention
- A healthy diet is primary prevention for COVID-19
- You should have a gut feeling about COVID-19
- Beyond dietary food patterns…plant-based compounds may mitigate COVID-19 risk
- Targeted nutrition support in the battle against COVID-19
- Targeted nutrition support in COVID-19: Armed with vitamin C
- Targeted nutrition support in COVID-19: In sync with zinc
- Targeted nutrition support in COVID-19: Micronutrients and phytonutrients are important players
- Optimal Takeaways for improving immunity and reducing susceptibility to COVID-19
- Optimal - The Podcast: Episode 8 -Blood Biomarkers and Risk Factors for COVID-19 and its Comorbidities
Some of the risk factors for COVID-19 include: [i] [ii] [iii] [iv] [v] [vi] [vii] [viii] [ix] [x] [xi] [xii] [xiii]
- Age
- Cardiovascular disease
- Dysbiosis
- Hyperglycemia
- Hypertension
- Immune system activation
- Inflammation
- Kidney disease
- Lack of fresh fruits and vegetables in the diet
- Obesity, especially abdominal/central obesity
- Oxidative stress
- Poverty
- Sedentary lifestyle, physical inactivity (also contribute to obesity)
- Toxin and pollution exposure
- Unhealthy Western-style diet
An unhealthy diet is a common denominator in many chronic diseases and even considered a leading cause of early death and disability.[xiv] On the other hand, a whole-foods plant-based diet is associated with:
- Healthy weight management
- Reduced ischemic heart disease and overall mortality
- Reduced reliance on medication
- Reduced risk and severity of obesity, inflammation, hyperglycemia, hyperlipidemia
- Reversal of advanced cardiovascular disease and type 2 diabetes
Researchers observe that in the wealthy nation of the United States, ”poor diet is the leading underlying cause of death,” even trumping tobacco use as a cause.[xv] Lack of nutrition education and limited access to fresh foods contribute to the epidemic of obesity and related morbidities including diabetes, hypertension, and heart disease. Along with darker skin (associated with vitamin D insufficiency), these comorbidities increase risk of more severe COVID-19 infections.
Metabolic disorders such as hypertension and diabetes cause chronic stress in the body, compromise immunity and even damage blood vessels. Chronic respiratory disease damages the lungs, making them more susceptible to infection and acute respiratory distress syndrome (ARDS) when challenged with viral exposure. The inflammatory response to viral infection can progress to systemic damage and possibly multi-organ failure. The virus itself may directly damage heart muscle while the associated cytokine storm may cause indirect cardiac damage. Elevations in AST, LDH, and creatinine indicate compromises in liver and kidney function.[xvi]
Abdominal or “central” obesity is a visual clue to underlying metabolic dysfunction and risk of hypertension and obesity. A cross-sectional study of 39 women at a metabolic syndrome clinic revealed: [xvii]
- 70% were obese
- 38% were hypertensive
- Abdominal circumference was 110.19 cm +/- 15.88 cm
- Triglycerides were 153.72 mg/dL +/- 7.07
- Fasting glucose was 188.6 mg/dL +/- 116
- Significant associations were found between
- Waist-to-height ratio and hypertension
- Visceral fat volume and diabetes
- Conicity Index and hypertension and diabetes
- Conicity Index calculated with Valdez formula with 1.18 cutoff point
Researchers point out that for COVID-19 patients younger than 60 years of age, those with a BMI of 30-34 were twice as likely to be admitted to acute care and 1.8 times more likely to be admitted to critical care units. Those with a BMI of 35 or above were 2.2 times more likely to be admitted to acute care and 3.6 times more likely to require critical care. It is noted that ~40% of the USA population has a BMI over 30.[xviii]
As you can see here, many of the comorbidities for severe COVID-19 are interrelated. They also share common causes, namely poor diet, compromised nutritional status, and suboptimal lifestyle habits. Each of these factors can be addressed with appropriate monitoring and lifestyle interventions which will be addressed in subsequent podcasts.
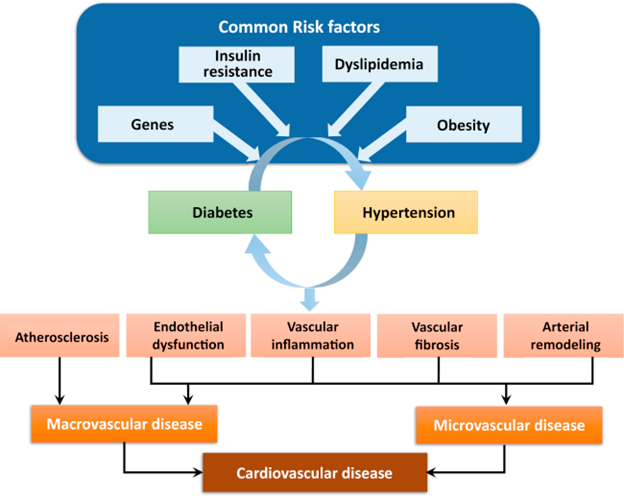
Source: Petrie, John R et al. “Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms.” The Canadian journal of cardiology vol. 34,5 (2018): 575-584. This is an open-access article under the CC BY license.
Next Up - Nutritional status and COVID-19: A covert factor in disease susceptibility
Research
[i] Tsoupras, Alexandros et al. “Inflammation, not Cholesterol, Is a Cause of Chronic Disease.” Nutrients vol. 10,5 604. 12 May. 2018.
[ii] Cena, Hellas, and Philip C Calder. “Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease.” Nutrients vol. 12,2 334. 27 Jan. 2020.
[iii] Hoffman, Jessie B, and Bernhard Hennig. “Protective influence of healthful nutrition on mechanisms of environmental pollutant toxicity and disease risks.” Annals of the New York Academy of Sciences vol. 1398,1 (2017): 99-107.
[iv] Shlisky, Julie et al. “Nutritional Considerations for Healthy Aging and Reduction in Age-Related Chronic Disease.” Advances in nutrition (Bethesda, Md.) vol. 8,1 17-26. 17 Jan. 2017.
[v] Hever, Julieanna, and Raymond J Cronise. “Plant-based nutrition for healthcare professionals: implementing diet as a primary modality in the prevention and treatment of chronic disease.” Journal of geriatric cardiology : JGC vol. 14,5 (2017): 355-368.
[vi] Hajat, Cother, and Emma Stein. “The global burden of multiple chronic conditions: A narrative review.” Preventive medicine reports vol. 12 284-293. 19 Oct. 2018.
[vii] Olivares, David E V et al. “Risk Factors for Chronic Diseases and Multimorbidity in a Primary Care Context of Central Argentina: A Web-Based Interactive and Cross-Sectional Study.” International journal of environmental research and public health vol. 14,3 251. 2 Mar. 2017.
[viii] Raghupathi, Wullianallur, and Viju Raghupathi. “An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach.” International journal of environmental research and public health vol. 15,3 431. 1 Mar. 2018.
[ix] Adams, Mary L et al. “The impact of key modifiable risk factors on leading chronic conditions.” Preventive medicine vol. 120 (2019): 113-118.
[x] Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 2020 Apr 8:S0033-0620(20)30077-3.
[xi] Petrie, John R et al. “Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms.” The Canadian journal of cardiology vol. 34,5 (2018): 575-584.
[xii] Barroso, Taianah Almeida, et al. "Association of central obesity with the incidence of cardiovascular diseases and risk factors." International Journal of Cardiovascular Sciences 30.5 (2017): 416-424.
[xiii] Hernández-Galdamez, Diego Rolando et al. “Increased Risk of Hospitalization and Death in Patients with COVID-19 and Pre-existing Noncommunicable Diseases and Modifiable Risk Factors in Mexico.” Archives of medical research vol. 51,7 (2020): 683-689.
[xiv] Hever, Julieanna, and Raymond J Cronise. “Plant-based nutrition for healthcare professionals: implementing diet as a primary modality in the prevention and treatment of chronic disease.” Journal of geriatric cardiology : JGC vol. 14,5 (2017): 355-368.
[xv] Belanger, Matthew J et al. “Covid-19 and Disparities in Nutrition and Obesity.” The New England journal of medicine vol. 383,11 (2020): e69.
[xvi] Zheng, Zhaohai et al. “Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis.” The Journal of infection vol. 81,2 (2020): e16-e25.
[xvii] Barroso, Taianah Almeida, et al. "Association of central obesity with the incidence of cardiovascular diseases and risk factors." International Journal of Cardiovascular Sciences 30.5 (2017): 416-424.
[xviii] Lighter, Jennifer et al. “Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission.” Clinical infectious diseases : an official publication of the Infectious Diseases Society of America vol. 71,15 (2020): 896-897.






