Vitamin D - You don’t know what you’re missing
Dicken Weatherby, N.D. and Beth Ellen DiLuglio, MS, RDN, LDN
Vitamin D3 (cholecalciferol), is produced in the skin from the cholesterol compound 7-dehydrocholesterol when exposed to UVB light from the sun. Cholecalciferol is then converted mainly by the liver to 25(OH) vitamin D and then by the kidney to active 1,25(OH)2 vitamin D. Total 25-OH vitamin D is commonly measured in the blood to assess vitamin D status.[i]
The ODX COVID-19 Series
- COVID-19: The pandemic that has become endemic
- COVID-19: Overlapping risk factors and chronic disease
- Nutritional status COVID-19: A covert factor in disease susceptibility
- COVID-19: Blood chemistry biomarker patterns - Clues and patterns lurking just under the surface
- COVID-19: Blood chemistry biomarker patterns - Down the research rabbit hole
- COVID-19: Blood Biomarkers - Neutrophils
- COVID-19: Blood Biomarkers - Albumin
- COVID-19: BloodBiomarkers - Cytokines
- COVID-19: Blood Biomarkers - Interleukin-6
- COVID-19: Blood Biomarkers - Interleukin-10
- COVID-19: Blood Biomarkers - Vitamin C
- COVID-19: Blood Biomarkers - Vitamin D
- COVID-19: Blood Biomarkers - Zinc
- Biomarker characteristics and blood type - help sharpen the COVID-19 clinical picture
- COVID-19: Initial indications and conventional interventions
- COVID-19: Long-term risk reduction - Naturopathic, functional medicine, and nutrition-based approaches to prevention
- A healthy diet is primary prevention for COVID-19
- You should have a gut feeling about COVID-19
- Beyond dietary food patterns…plant-based compounds may mitigate COVID-19 risk
- Targeted nutrition support in the battle against COVID-19
- Targeted nutrition support in COVID-19: Armed with vitamin C
- Targeted nutrition support in COVID-19: In sync with zinc
- Targeted nutrition support in COVID-19: Micronutrients and phytonutrients are important players
- Optimal Takeaways for improving immunity and reducing susceptibility to COVID-19
- Optimal - The Podcast: Episode 8 -Blood Biomarkers and Risk Factors for COVID-19 and its Comorbidities
Sun exposure, which could provide 80-100% of vitamin D requirements under optimal conditions, is often insufficient due to latitude, winter season, clothing, indoor living, weather, dark skin (melanin in dark skin blocks UV light, and vitamin D production), etc. Also, cutaneous production of vitamin D may decline with age.[ii]
Historically, exposure to sunlight during the spring and summer months would lead to an accumulation of vitamin D in adipose tissue. Subsequently in the winter when food was scarce and weight loss ensued, stored vitamin D was released, helping to maintain adequate serum levels. In modern times an overabundance of food prevents that weight loss and endogenous release of vitamin D, contributing to deficiency.[iii]
Vitamin D insufficiency is emerging as a significant factor in COVID-19 susceptibility and progression due to its various roles as an anti-inflammatory, antifibrotic, antioxidant, and immune-modulating compound.[iv] Research suggests that a 25(OH)D level of 30 ng/mL (75 nmol/L) or greater was associated with reduced disease severity and mortality.[v]
Insufficiency or deficiency of vitamin D:
- Impairs innate immunity and increases vulnerability to viral disease
- Increases renin-angiotensin system and susceptibility to COVID-19 cytokine storm
- Groups at higher risk for vitamin D deficiency are the same groups at higher risk for severe COVID-19:[vi]
- Chronic disease: cardiovascular disease, diabetes, hypertension)
- Dark-skinned (high in melanin)
- Elderly
- Hypertension
- Institutional living
- Lack of sun exposure
- Males
- Obesity
- COVID-19 fatality parallels rate of vitamin D deficiency
- Symptomatic patients who were Vitamin D deficient (11.1 ng/mL) were significantly likely to test PCR positive for SARS-Co-V-2 compared to symptomatic patients with vitamin D levels of 24.6 ng/mL who ultimately tested negative.
A hospital study of 134 COVID-19 patients noted that only 19% of ICU COVID patients had a vitamin D level above 20 ng/mL (50 nmol/L). Researchers note that vitamin D deficiency is common in critically ill patients and is associated with acute respiratory distress syndrome due to exacerbation of lung inflammation.[vii]
A study of 50 hospitalized mild to severe COVID-19 patients revealed vitamin D levels significantly lower than those of controls. Approximately 76% of patients presented with vitamin D insufficiency with levels of 20 ng/mL (50 nmol/L) or less. Severe vitamin D deficiency with levels 10 ng/mL (25 nmol/L) or less was observed in 24% of patients versus 7.3% of controls. Selenium deficiency was also observed in 42% of patients with mean levels of 103.2 ug/L (1.31 umol/L) in males and 96.7 ug/L (1.23 umol/L) in females.[viii]
Researchers emphasize the importance of assessing and addressing insufficiencies in micronutrients including vitamin C, vitamin D, and selenium in in COVID-19 patients.[ix]
Inflammatory markers in relation to Vitamin D[x]
|
Parameter |
Patients with Serum 25 (OH) D level) > 20 ng/mL n = 64 [X] |
Patients with Serum 25 (OH) D level) < 20 ng/mL n = 90 [Y] |
‘p’ value |
|
Group A Asymptomatic COVID-19 |
62 |
29 |
NA |
|
Group B Critically Ill COVID-19 |
2 |
61 |
NA |
|
Serum IL-6 in pg/mL (mean ± 2SD) |
12.18 ± 4.29 |
19.34 ± 6.17 |
0.03* |
|
Serum TNF α in pg/mL (mean ± 2SD) |
11.87 ± 3.15 |
13.26 ± 5.64 |
0.06* |
|
Serum ferritin in ng/mL (mean ± 2SD) |
186.83 ± 20.18 |
319.17 ± 38.21 |
0.0003* |
*Chi-square test. SD Standard deviation.
The mean concentration (in ng/mL) of 25 (OH)D in Group A was 27.89 ± 6.21where as in Group B the mean level was 14.35 ± 5.79.
The analysis of serum level of inflammatory markers reveals mean IL-6 level (in pg/mL) of 19.34 ± 6.17 in patients with vitamin D deficiency (serum 25 (OH)D < 20 ng/mL) and 12.18 ± 4.29 in patients with normal vitamin D level, the difference was found to be statistically significant. Serum ferritin level was also significantly high in patients with vitamin D deficiency (319.17 ± 38.21 ng/mL vs 186.83 ± 20.18 ng/mL) than in patients with normal vitamin D. Serum TNFα level (in pg/mL) was also high in vitamin D deficient COVID-19 patients (13.26 ± 5.64 vs 11.87 ± 3.15) but the difference was not significant. Among both, the group's diabetes was the commonest co-morbidity followed by hypertension.
Source: Jain, Anshul et al. “Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers.” Scientific reports vol. 10,1 20191. 19 Nov. 2020, doi:10.1038/s41598-020-77093-z Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. http://creativecommons.org/licenses/by/4.0/.
Classification of vitamin D levels (serum 25(OH)D levels):
|
Classification |
Nanograms |
Nanomoles |
Recommended D intake |
|
Danger of toxicity |
>100 ng/ml* |
>250 nmol/l |
|
|
Normal or optimal |
>30 ng/ml |
>75 nmol/l |
400–4,000 IU/day |
|
Insufficient |
21–29 ng/ml |
51–74 nmol/l |
4,000–6,000 IU/day |
|
Deficient |
11–20 ng/ml |
26–50 nmol/l |
7,000 IU/day |
|
Severely deficient (often not distinguished from deficient) |
<10 ng/ml |
25 nmol/l |
10,000 IU/day x 1 month or 500,000 IU x 1 |
|
NIH target |
30 ng/mL |
75 nmol/L |
2000 IU/day |
|
Prevention of respiratory infection |
40-60 ng/mL |
100-150 nmol/L |
6000 IU/day normal weight until goal 7000-8000/day obese |
|
Reduce risk CVD, hypertension |
50-80 ng/mL |
125-200 nmol/L |
4000-10000 IU/day until goal |
|
COVID-19 |
40-60 ng/mL |
100-150 nmol/L |
5000-10000 IU/day until goal |
*some sources found that 150 ng/ml was not harmful.
Source: Benskin, Linda L. “A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency.” Frontiers in public health vol. 8 513. 10 Sep. 2020, doi:10.3389/fpubh.2020.00513 This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
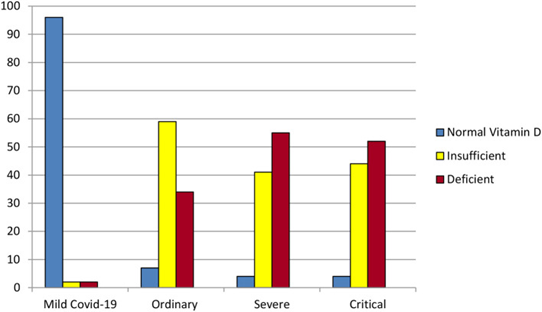 Some of the results of the retrospective chart review by Alipio et al. (3). Of the 212 hospitalized COVID-19 patients, 96% of those with mild COVID-19 had normal vitamin D levels (above 30 ng/ml). In contrast, over 50% of the patients with severe or critical COVID-19 were vitamin D deficient (level 20 ng/ml or lower).
Some of the results of the retrospective chart review by Alipio et al. (3). Of the 212 hospitalized COVID-19 patients, 96% of those with mild COVID-19 had normal vitamin D levels (above 30 ng/ml). In contrast, over 50% of the patients with severe or critical COVID-19 were vitamin D deficient (level 20 ng/ml or lower).
Source: Benskin, Linda L. “A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency.” Frontiers in public health vol. 8 513. 10 Sep. 2020, doi:10.3389/fpubh.2020.00513 This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
A prospective observational study assessed serum levels of 25(OH) vitamin D, as well as markers of inflammation (IL-6, ferritin, TNF-alpha) in Indian COVID-19 patients. Of 154 patients, 91 patients were asymptomatic (Group A) and 63 patients were severely ill and required ICU care (Group B).[xi] Data indicates that vitamin D deficiency was significantly related to severe COVID-19, and also correlated with elevations in IL-6, ferritin, TNF-a, and fatality rates:
Mild vs severe COVID-19
| Group A (asymptomatic) | Group B (symptomatic) | |
| Vitamin D, mean | 27.89 ng/mL | 14.35 ng/mL highly significant |
| Vitamin D deficiency | 32.96% | 96.82% |
Vitamin D deficient vs sufficient:
| Additional Biomarkers | Vitamin D deficient | Vitamin D sufficient |
| IL-6 | 19.34 pg/mL | 12.18 pg/mL |
| Ferritin | 319.17 ng/mL | 186.83 ng/mL |
| TNF-alpha | 13.26 pg/mL | 11.87 pg/mL |
| Fatality | 21% | 31% |
Standard reference range 25(OH) vitamin D
Quest Diagnostics[xii] 30-100 ng/mL
Labcorp[xiii] 30-100 ng/mL
As pointed out by Grant et al. 2020, the goal of vitamin D therapy should be to maintain serum 25(OH)D concentrations of at least 40-60 ng/mL (100-150 nmol/L). For those at risk of COVID-19 or influenza, 10,000 IU/day of vitamin D3 may be indicated for two weeks followed by 5,000 IU/day until goals are reached.[xiv] Researchers note that higher levels of supplementation may be useful for those already infected with the virus.
A literature review of randomized trials, systematic reviews, meta-analyses, and international consensus conferences confirms maintenance of robust serum vitamin 25(OH)D levels in the range of 50-70 ng/mL (125-175 nmol/L).[xv]
Remember, it is uber important not to forget to check vitamin D levels and address insufficiencies early on in order to mount the best defense against COVID-19.
Next Up - COVID-19: Blood Biomarkers - Zinc
Research
[i] Bikle, Daniel. “Vitamin D: Production, Metabolism, and Mechanisms of Action.” Endotext, edited by Kenneth R Feingold et. al., MDText.com, Inc., 11 August 2017.
[ii] Richardson, David P, and Julie A Lovegrove. “Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective.” The British journal of nutrition, 1-7. 20 Aug. 2020, doi:10.1017/S000711452000330X
[iii] Benskin, Linda L. “A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency.” Frontiers in public health vol. 8 513. 10 Sep. 2020, doi:10.3389/fpubh.2020.00513
[iv] Jain, Anshul et al. “Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers.” Scientific reports vol. 10,1 20191. 19 Nov. 2020, doi:10.1038/s41598-020-77093-z
[v] Maghbooli, Zhila et al. “Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection.” PloS one vol. 15,9 e0239799. 25 Sep. 2020, doi:10.1371/journal.pone.0239799
[vi] Benskin, Linda L. “A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency.” Frontiers in public health vol. 8 513. 10 Sep. 2020, doi:10.3389/fpubh.2020.00513
[vii] Alexander, Jan et al. “Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19.” Nutrients vol. 12,8 2358. 7 Aug. 2020, doi:10.3390/nu12082358
[viii] Im, Jae Hyoung et al. “Nutritional status of patients with COVID-19.” International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases vol. 100 (2020): 390-393. doi:10.1016/j.ijid.2020.08.018
[ix] Bae, Minkyung, and Hyeyoung Kim. “Mini-Review on the Roles of Vitamin C, Vitamin D, and Selenium in the Immune System against COVID-19.” Molecules (Basel, Switzerland) vol. 25,22 5346. 16 Nov. 2020, doi:10.3390/molecules25225346
[x] Jain, Anshul et al. “Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers.” Scientific reports vol. 10,1 20191. 19 Nov. 2020, doi:10.1038/s41598-020-77093-z
[xi] Jain, Anshul et al. “Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers.” Scientific reports vol. 10,1 20191. 19 Nov. 2020, doi:10.1038/s41598-020-77093-z
[xii] Quest Diagnostics 25-hydroxy vitamin D.
[xiii] Labcorp. 25-hydroxy vitamin D.
[xiv] Grant WB, Lahore H, McDonnell SL, et al. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020 Apr 2;12(4). pii: E988. doi: 10.3390/nu12040988. Review. PubMed PMID: 32252338.
[xv] Zotarelli Filho, Idiberto José, et al. “Major Meta-Analysis, Randomized Clinical Studies, and International Consensus on Serum Levels and Importance of Supplementing Vitamin D:State of the Art.” MedNEXT Journal of Medical and Health Sciences, 2021, pp. 54–66., doi:10.34256/mdnt2129.






