Some blood biomarkers and related clues are associated with the potential causes of kidney stones, also known as nephrolithiasis or urolithiasis.
The kidneys and lungs are responsible for maintaining the body's acid-base balance. The lungs excrete volatile acidic carbon dioxide, while the kidneys excrete non-volatile metabolic acids and reabsorb alkaline bicarbonate. These help keep blood pH at an optimal 7.35 – 7.45. Low-grade metabolic acidosis and overt metabolic acidosis (serum bicarbonate below 22 mmol/L) increase the risk of kidney stone formation (Wieers 2024).
The most common kidney stones are composed of calcium oxalate, followed by calcium phosphate, uric acid, struvite, and cystine (Chmiel 2023).
Kidney stone formation is associated with a significantly increased risk of cardiovascular disease, likely related to underlying mechanisms, including vascular calcification, oxidative stress, endothelial dysfunction, and cholesterol-induced pathology (Muschialli 2024). Kidney stone formation has been associated with a 20-24% increased risk of CVD, myocardial infarction, and stroke (Saenz-Medina 2022).
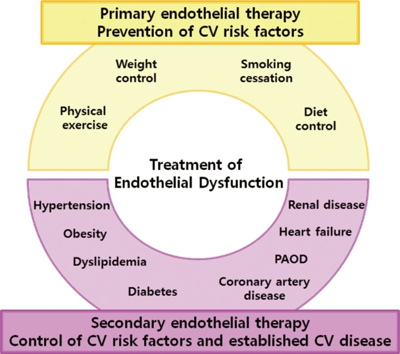
Therapeutic approaches to endothelial dysfunction. Endothelial therapy can be achieved with primary endothelial therapy for prevention of healthy endothelial function by controlling cardiovascular risk factors and secondary endothelial therapy for to improve dysfunctional endothelial homeostasis by treating underlying cardiovascular risk factors and cardiovascular disease. CV, cardiovascular; PAOD, peripheral arterial occlusive disease.
Source: Park, Kyoung-Ha, and Woo Jung Park. “Endothelial Dysfunction: Clinical Implications in Cardiovascular Disease and Therapeutic Approaches.” Journal of Korean medical science vol. 30,9 (2015): 1213-25. doi:10.3346/jkms.2015.30.9.1213 This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
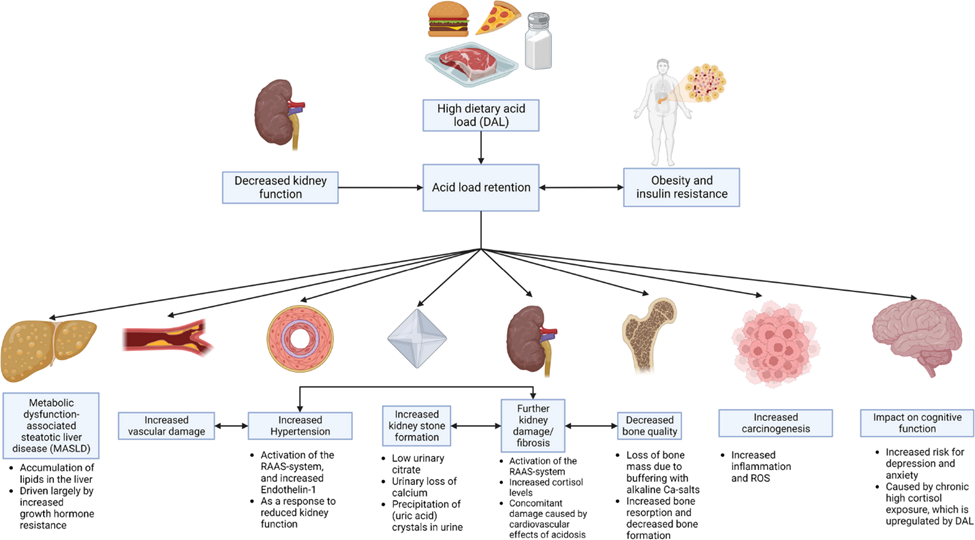
Source: Wieers, Michiel L A J et al. “Dietary acid load in health and disease.” Pflugers Archiv : European journal of physiology, 10.1007/s00424-024-02910-7. 29 Jan. 2024, doi:10.1007/s00424-024-02910-7 This article is licensed under a Creative Commons Attribution 4.0 International License
CLICK HERE to learn more about Alkalizing the Urine
Chmiel, John A et al. “Vitamins as regulators of calcium-containing kidney stones - new perspectives on the role of the gut microbiome.” Nature reviews. Urology vol. 20,10 (2023): 615-637. doi:10.1038/s41585-023-00768-5
Di, Xingpeng et al. “Association between the systemic immune-inflammation index and kidney stone: A cross-sectional study of NHANES 2007-2018.” Frontiers in immunology vol. 14 1116224. 21 Feb. 2023, doi:10.3389/fimmu.2023.1116224
Khan, Saeed R et al. “Kidney stones.” Nature reviews. Disease primers vol. 2 16008. 25 Feb. 2016, doi:10.1038/nrdp.2016.8
Liang, Dan et al. “The association between C-reactive protein levels and the risk of kidney stones: a population-based study.” BMC nephrology vol. 25,1 39. 27 Jan. 2024, doi:10.1186/s12882-024-03476-3
Mao, Weipu et al. “Neutrophil-lymphocyte ratio acts as a novel diagnostic biomarker for kidney stone prevalence and number of stones passed.” Translational andrology and urology vol. 10,1 (2021): 77-86. doi:10.21037/tau-20-890
Muschialli, Luke et al. “Epidemiological and biological associations between cardiovascular disease and kidney stone formation: A systematic review and meta-analysis.” Nutrition, metabolism, and cardiovascular diseases : NMCD vol. 34,3 (2024): 559-568. doi:10.1016/j.numecd.2023.09.011
Nojaba, Leila. and Nilmarie Guzman. “Nephrolithiasis.” StatPearls, StatPearls Publishing, 8 August 2023.
Saenz-Medina, Javier et al. “Endothelial Dysfunction: An Intermediate Clinical Feature between Urolithiasis and Cardiovascular Diseases.” International journal of molecular sciences vol. 23,2 912. 14 Jan. 2022, doi:10.3390/ijms23020912
Tanaka, Yoshimi et al. “The influence of serum uric acid on renal function in patients with calcium or uric acid stone: A population-based analysis.” PloS one vol. 12,7 e0182136. 31 Jul. 2017, doi:10.1371/journal.pone.0182136
Wei, Baian et al. “Association between drinking status and risk of kidney stones among United States adults: NHANES 2007-2018.” BMC public health vol. 24,1 820. 15 Mar. 2024, doi:10.1186/s12889-024-18307-1
Wieers, Michiel L A J et al. “Dietary acid load in health and disease.” Pflugers Archiv : European journal of physiology, 10.1007/s00424-024-02910-7. 29 Jan. 2024, doi:10.1007/s00424-024-02910-7
Wu, Jing et al. “Association Between Serum Magnesium and the Prevalence of Kidney Stones: a Cross-sectional Study.” Biological trace element research vol. 195,1 (2020): 20-26. doi:10.1007/s12011-019-01830-3
Yen, Yunhe et al. “Heavy Metal Components in Blood and Urinary Stones of Urolithiasis Patients.” Biological trace element research vol. 185,2 (2018): 266-274. doi:10.1007/s12011-018-1253-x
Zhao, Enyang et al. “Intestinal dysbacteriosis leads to kidney stone disease.” Molecular medicine reports vol. 23,3 (2021): 180. doi:10.3892/mmr.2020.11819